Physical health
Physical health is a basic building block for children’s current wellbeing and future life outcomes. Being physically healthy includes being physically active, having a good diet and being in the healthy weight range.
Children aged 6 to 11 years are in a critical phase for establishing positive health behaviours to support wellbeing outcomes over their lifetime.
Last updated August 2021
Some data is available on whether WA children aged 6 to 11 years are physically healthy.
Overview
This indicator considers key measures of physical health for children including physical activity, screen time, diet, weight and long-term health issues.
Physical health is influenced by a range of factors including genetic, social and environmental influences. Research has found that Australian children living in areas with a high risk of social exclusion1 have, on average, worse health outcomes than children living in other areas.2 In particular, socioeconomic indicators such as having higher income and education levels are linked to better health outcomes.3
In the Commissioner’s 2019 Speaking Out Survey, nearly two-thirds of Year 4 to Year 6 students rated their health as excellent or very good (26.8% excellent and 36.9% very good), and another 28.7 per cent rated their health as good.
While less than half of WA children aged five to nine years were assessed by their parent/carer as meeting the recommended level of physical activity in 2019, the proportion of children that parents/carers reported as meeting the recommendation continued to increase from 37.6 per cent in 2015 to 48.0 per cent in 2019.
There is limited recent data, however the available data suggests that Aboriginal children are more physically active than non-Aboriginal children in WA.
Areas of concern
In 2019 the proportion of WA children aged nine to 15 years eating sufficient vegetables remains very low at 7.6 per cent, however this is a modest increase from 4.1 per cent in 2017.
Only 32.3 per cent of WA female children and young people aged 5 to 15 years were reported as meeting the physical activity guidelines, compared to 45.2 per cent of male WA children and young people.
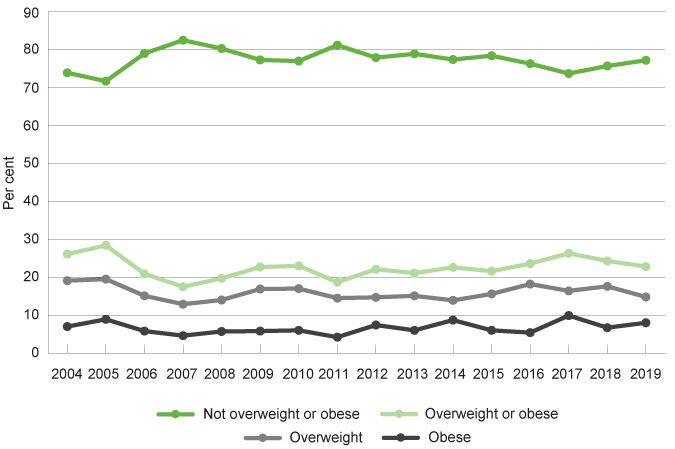
Nearly one-quarter (22.8%) of WA children and young people aged 5 to 15 years were overweight or obese in 2019.
Proportion of children and young people aged 5 to 15 years by BMI categories, per cent, WA, 2004 to 2019
Dombrovskaya M et al 2020, Health and Wellbeing of Children in Western Australia in 2019, Overview and Trends, WA Department of Health (and previous years’ reports)
There is no data publicly available on the physical health of the 1,906 children aged six to 11 years in care in WA. Furthermore, in 2015, only 53.1 per cent of children entering out-of-home care had a medical assessment, as required by Departmental guidelines.
Endnotes
- In this research social exclusion comprised five domains: socioeconomic circumstances, education, connectedness, housing and health service access.
- Australian Institute of Health and Welfare (AIHW) and National Centre for Social and Economic Modelling (NATSEM) 2014, Child social exclusion and health outcomes: A study of small areas across Australia, Bulletin 121, June 2014.
- World Health Organisation (WHO) 2008, Closing the gap in a generation: health equity through action on the social determinants of health - Final report of the commission on social determinants of health, WHO.
Last updated August 2021
Being physically healthy is critical for children’s wellbeing as many health conditions in adulthood have their origins in childhood.1 Good health also influences children’s engagement with family, education and friends and supports socio-emotional health.2
In 2019, the Commissioner conducted the Speaking Out Survey (SOS19) which sought the views of a broadly representative sample of 4,912 Year 4 to Year 12 students in WA on factors influencing their wellbeing, including a range of questions on physical health.3
Almost two-thirds (63.7%) of Year 4 to Year 6 students rated their health as excellent or very good (26.8% excellent and 36.9% very good) while 7.6 per cent said their health was only fair or poor (6.9% fair and 0.7% poor).
|
Male |
Female |
Metropolitan |
Regional |
Remote |
All |
|
|
Excellent |
28.8 |
25.2 |
26.6 |
29.3 |
22.6 |
26.8 |
|
Very good |
33.4 |
40.1 |
38.8 |
28.9 |
36.3 |
36.9 |
|
Good |
28.7 |
29.0 |
26.8 |
34.1 |
34.7 |
28.7 |
|
Fair |
8.2 |
5.5 |
7.0 |
6.7 |
5.8 |
6.9 |
|
Poor |
0.9 |
N/A |
0.7 |
N/A |
N/A |
0.7 |
Source: Commissioner for Children and Young People WA 2020, Speaking Out Survey 2019 Data Tables [unpublished]
There were no significant differences between male and female Year 4 to Year 6 students’ health ratings or between students in regional, remote or metropolitan locations.
Aboriginal and non-Aboriginal Year 4 to Year 6 students also reported similar health ratings.
|
Aboriginal |
Non-Aboriginal |
|
|
Excellent |
28.5 |
26.7 |
|
Very Good |
27.6 |
37.7 |
|
Good |
35.9 |
28.1 |
|
Fair |
7.1 |
6.9 |
|
Poor |
0.9 |
0.7 |
Source: Commissioner for Children and Young People WA 2020, Speaking Out Survey 2019 Data Tables [unpublished]
Having a good nights’ sleep is increasingly being recognised as critical for physical and mental health.4 For physical health, inadequate sleep is associated with a higher risk of children becoming overweight and having poorer overall health.5,6
The recommended hours of sleep is nine to 11 hours for children aged five to 13 years.7
SOS19 asked children what time they usually went to sleep on a school night and what time they usually woke up on a school day. Most students in Years 4 to 6 reported usually going to sleep by 9pm (73.8%) on a school night and waking up by 8am (97.3%) on a school day.8
Around one-third (31.3%) of children in Years 4 to 6 went to sleep before 8pm, and over 90 per cent (91.5%) reported they usually went to sleep before 10pm.
|
Male |
Female |
Metropolitan |
Regional |
Remote |
All |
|
|
Before 8pm |
31.0 |
31.1 |
28.5 |
38.8 |
43.0 |
31.3 |
|
8pm to 8:59pm |
42.0 |
43.5 |
43.4 |
40.8 |
36.9 |
42.5 |
|
9pm to 9:59pm |
17.1 |
18.2 |
19.2 |
13.6 |
10.7 |
17.7 |
|
10pm to 10:59pm |
5.9 |
5.1 |
6.2 |
2.4 |
6.5 |
5.6 |
|
11pm to 11:59pm |
1.6 |
1.0 |
1.1 |
1.7 |
1.8 |
1.3 |
|
After midnight |
2.4 |
1.1 |
1.6 |
2.6 |
1.1 |
1.7 |
Source: Commissioner for Children and Young People WA 2020, Speaking Out Survey 2019 Data Tables [unpublished]
A low, but significantly greater proportion of male children than female children went to sleep after midnight (male: 2.4%, female: 1.1%).
There were also differences based on where students lived – with a significantly greater proportion of children in both regional (38.8%) and remote (43.0%) locations going to sleep before 8pm, compared with children in metropolitan areas (28.5%).
Recent research based on the Longitudinal study of Australian Children found that at least 88 per cent of children aged 6 to 11 years met the minimum sleep requirements on a school night.9
This study concluded that children who did not meet the minimum guidelines for sleep were more likely to have poor mental health, be late or absent from school, spend more time on homework and more time on the internet.10
Endnotes
- Australian Institute of Health and Welfare (AIHW) 2011, Young Australians: their health and wellbeing 2011, AIHW, p. 1.
- Australian Institute of Health and Welfare (AIHW) 2020, Australia’s Children, AIHW, p. 30.
- Commissioner for Children and Young People WA 2020, Speaking Out Survey: The views of WA children and young people on their wellbeing - a summary report, Commissioner for Children and Young People WA.
- Evans-Whipp T & Gasser C 2019, Are children and adolescents getting enough sleep? In LSAC Annual Statistical Report 2018, Australian Institute of Family Studies, p. 29.
- Landhuis CE et al 2008, Childhood sleep time and long-term risk for obesity: A 32-year prospective birth cohort study, Pediatrics, Vol 122, No 5.
- Chaput J et al 2016, Systematic review of the relationships between sleep duration and health indicators in school-aged children and youth, Applied physiology, nutrition and metabolism, Vol 41 (6 Suppl 3).
- Department of Health 2020, Australian 24-Hour Movement Guidelines for Children and Young People (5-17 years) – An Integration of Physical Activity, Sedentary Behaviour and Sleep, Australian Government.
- Commissioner for Children and Young People WA 2020, Speaking Out Survey: The views of WA children and young people on their wellbeing - a summary report, Commissioner for Children and Young People WA, p. 34.
- Ibid, p. 35.
- Ibid, p. 29.
Last updated August 2021
Physical activity makes an important positive contribution to the health and wellbeing of children. Doing regular moderate and/or vigorous physical activity supports the development of healthy bones, muscles, joints and a healthy cardiovascular system. It is also an important element to achieving and maintaining a healthy weight.
Physical activity also enhances cognitive functioning including memory, concentration and the ability to learn.1 Furthermore, it is associated with social and emotional benefits in childhood, including self-regulation and improved self-esteem.2
The current recommendation for physical activity is that children aged five to 12 years should do at least 60 minutes of moderate to vigorous intensity physical activity every day, including at least three days per week where the activities strengthen muscle and bone.3
Data collected on children’s physical activity is often survey-based information, either self-reported daily physical activity or parent-reported daily physical activity. This measure reports data from three key data sources:
- The Commissioner’s 2019 Speaking Out Survey
- WA Department of Health, Health and Wellbeing Surveillance System
- Australian Bureau of Statistics, National Health Survey
In 2019, the Commissioner conducted the Speaking Out Survey (SOS19) which sought the views of a broadly representative sample of 4,912 Year 4 to Year 12 students in WA on factors influencing their wellbeing, including a range of questions on physical health.4
In this survey, 66.0 per cent of Year 4 to Year 6 students reported they cared very much about staying fit and being physically active, while 23.6 per cent cared some. Just over 10 per cent of students cared a little (7.8%) or not at all (2.6%).
|
Male |
Female |
Metropolitan |
Regional |
Remote |
All |
|
|
Very much |
66.3 |
65.0 |
66.9 |
64.7 |
59.6 |
66.0 |
|
Some |
21.6 |
26.0 |
23.0 |
24.4 |
28.6 |
23.6 |
|
A little |
8.9 |
6.9 |
7.9 |
6.9 |
9.4 |
7.8 |
|
Not at all |
3.2 |
2.1 |
2.3 |
4.0 |
2.4 |
2.6 |
Source: Commissioner for Children and Young People WA 2020, Speaking Out Survey 2019 Data Tables [unpublished]
Year 4 to 6 students were significantly more likely than high school students to report they cared very much about staying fit and physically active (66.0% compared to 50.8%). For more information refer to the Adequate physical activity measure for the 12 to 17 years age group.
In particular, female students in primary school were significantly more likely than female students in high school to report they cared very much about staying fit and physically active (65.0% compared to 46.1%).
It should be noted that this data is from different cohorts of students in primary school and high school. Younger children may be influenced by more public awareness of the importance of healthy eating through increased public health messaging and advertising (e.g. graphic advertising of the damaging effects of sugary drinks) and a greater focus in schools on healthy eating. Results from future Speaking Out Surveys will show changes over time and determine whether this primary school cohort continue to care more about staying fit and physically active as they move into high school – or if the transition into high school and through adolescence changes students’ views.
There were no significant differences in responses regarding caring about staying fit or physically active between Year 4 to Year 6 students in metropolitan, regional and remote locations.
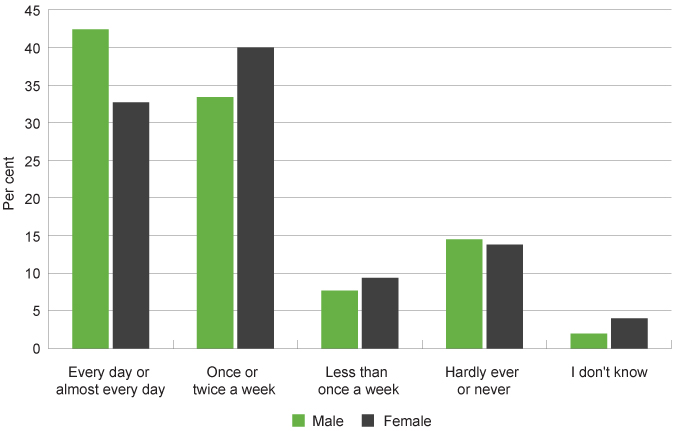
Students in SOS19 were also asked how often they usually spend time practising or playing a sport (like footy training, gymnastics, swimming) outside of school.
Nearly a quarter (22.6%) of Year 4 to Year 6 students said they practise or play a sport outside of school less than once a week or hardly ever or never. Just under thirty-eight per cent said they spend time practising or playing a sport every day or almost every day outside of school, while a similar proportion (36.4%) said they do this once or twice a week.
|
Male |
Female |
Metropolitan |
Regional |
Remote |
All |
|
|
Every day or almost every day |
42.4 |
32.7 |
38.7 |
34.7 |
37.1 |
37.9 |
|
Once or twice a week |
33.4 |
40.0 |
36.4 |
36.0 |
37.0 |
36.4 |
|
Less than once a week |
7.7 |
9.4 |
7.8 |
10.5 |
10.1 |
8.4 |
|
Hardly ever or never |
14.5 |
13.8 |
14.4 |
15.1 |
10.4 |
14.2 |
|
I don't know |
2.0 |
4.0 |
2.8 |
3.7 |
5.3 |
3.1 |
Source: Commissioner for Children and Young People WA 2020, Speaking Out Survey 2019 Data Tables [unpublished]
Proportion of Year 4 to Year 6 students reporting how much time they spend practising or playing a sport outside of school by gender, per cent, WA, 2019
Source: Commissioner for Children and Young People WA 2020, Speaking Out Survey 2019 Data Tables [unpublished]
Female students were significantly less likely than male students to play or practise a sport every day or almost every day outside of school (32.7% compared to 42.4%).
These results are consistent with research reporting that male children and young people are more likely to do more physical activity than female children and young people.5,6
Further analysis of the SOS19 data shows that there is a statistically significant relationship between children in Years 4 to 6 caring a lot about staying fit and being physically active and the time they spend practising or playing a sport outside of school.
There were no significant differences between Year 4 to Year 6 students in metropolitan, regional and remote locations practising or playing sport outside of school.
The WA Department of Health administers the Health and Wellbeing Surveillance System to monitor the health of WA’s general population, which includes interviewing WA parents and carers about the health of their children aged 0 to 15 years.7 In this survey, parents and carers are asked about their children’s activity levels and based on these responses, the Department of Health determine the proportion of WA children meeting the physical activity guidelines.
Research shows that while parent-reported data on physical activity for children under 12 years of age is valid, it has limitations depending on the questions asked (e.g. difficulty estimating unstructured play).8
|
No activity |
1 to 6 sessions |
7 or more sessions |
7 or more sessions |
|
|
2012 |
2.8 |
27.0 |
19.6 |
50.6 |
|
2013 |
5.4* |
28.9 |
21.8 |
43.9 |
|
2014 |
7.5* |
27.6 |
25.1 |
39.8 |
|
2015 |
N/A |
31.0 |
30.3 |
37.6 |
|
2016 |
N/A |
30.4 |
24.7 |
43.2 |
|
2017 |
2.5* |
31.4 |
19.3 |
46.7 |
|
2018 |
8.4* |
23.0 |
22.3 |
46.3 |
|
2019 |
3.6* |
29.3 |
19.1 |
48.0 |
Source: Dombrovskaya M et al 2020, Health and Wellbeing of Children in Western Australia in 2019, Overview and Trends. Department of Health, Western Australia (and previous years’ reports) 9
* Prevalence estimate has a relative standard error of 25 per cent to 50 per cent and should be used with caution.
N/A Prevalence estimate has a relative standard error greater than 50 per cent and is considered too unreliable for general use.
From 2012 to 2015, there was a decline in children aged five to nine years being assessed as meeting the recommended activity level, however from 2016 the proportion of children meeting the recommendation has gradually increased. In 2019, still less than half (48.0%) of WA children aged five to nine years were assessed by their parent/carer as meeting the recommended level of activity.
In 2011–12, the Australian Bureau of Statistics (ABS) conducted the National Nutrition and Physical Activity Survey (NNPAS) as part of the Australian Health Survey.10 In this survey, parents were asked about their child’s previous week’s physical activity and data was collected by jurisdiction.11 Results showed that the proportion of WA children and young people aged two to 17 years meeting the physical activity recommendations in 2011–12 was very low (32.5%), although this was in line with other states and territories in Australia.
In 2017–18, the Australian Bureau of Statistics conducted the National Health Survey, in this survey they reported on the physical activity of young people and adults aged 15 years and over. This survey did not consider children under 15 years of age.
Data and research has consistently found that male children are more likely to do more physical activity than female children.12,13
Consistent with the SOS19 data, the WA Health and Wellbeing Surveillance System reports that a higher proportion of male children and young people than female children and young people generally meet the recommended activity level.14
|
Male |
Female |
|
|
2012 |
55.0 |
42.7 |
|
2013 |
49.1 |
33.6 |
|
2014 |
39.8 |
40.3 |
|
2015 |
48.5 |
28.0 |
|
2016 |
39.9 |
39.5 |
|
2017 |
46.2 |
32.5 |
|
2018 |
45.4 |
34.5 |
|
2019 |
45.2 |
32.3 |
Source: Dombrovskaya M et al 2020, Health and Wellbeing of Children in Western Australia in 2019, Overview and Trends, WA Department of Health (and previous years’ reports) 15
In 2008, researchers from Edith Cowan University and the University of WA conducted the Child and Adolescent Physical Activity and Nutrition Survey (CAPANS) in WA.16 In this study participants wore pedometers and completed exercise diaries. The researchers found significant differences between male and female respondents. While only 41.2 per cent of male primary school students reported activity that met the recommended guidelines, even fewer female primary school students (27.4%) reported activity that met the recommended guidelines.17 This survey has not been repeated.
Aboriginal children
There is limited regularly reported data on the physical activity of WA Aboriginal children or children in metropolitan, regional and remote locations. The WA Health and Wellbeing Surveillance System does not provide disaggregated information on physical activity for Aboriginal children or by geographic location.
In SOS19, a marginally lower proportion of Aboriginal Year 4 to Year 6 students than non-Aboriginal students reported they cared very much about staying fit or physically active (Aboriginal: 62.7%, non-Aboriginal 66.3%).
|
Aboriginal |
Non-Aboriginal |
|
|
Very much |
62.7 |
66.3 |
|
Some |
22.8 |
23.7 |
|
A little |
9.9 |
7.6 |
|
Not at all |
4.6 |
2.4 |
Source: Commissioner for Children and Young People WA 2020, Speaking Out Survey 2019 Data Tables [unpublished]
However, Aboriginal students were more likely to practise or play a sport every day (44.4% compared to 37.4%).
|
Aboriginal |
Non-Aboriginal |
|
|
Every day or almost every day |
44.4 |
37.4 |
|
Once or twice a week |
29.7 |
36.9 |
|
Less than once a week |
8.1 |
8.5 |
|
Hardly ever or never |
9.2 |
14.6 |
|
I don't know |
8.6 |
2.7 |
Source: Commissioner for Children and Young People WA 2020, Speaking Out Survey 2019 Data Tables [unpublished]
This is consistent with other data that suggests WA Aboriginal children and young people are generally more physically active than non-Aboriginal children and young people in WA.
In 2012–13, the ABS conducted the Australian Aboriginal and Torres Strait Islander Health Survey: Physical activity. They reported that a higher proportion of WA Aboriginal children and young people (45.6%) aged five to 17 years in non-remote areas met the physical activity recommendation compared with non-Aboriginal children and young people (40.5%).18
In remote areas across Australia,19 over four in five (86%) Aboriginal children aged five to eight years and an equivalent proportion of nine to 11 year olds (87%) did more than 60 minutes of physical activity on the day prior to the interview. 20
There is no information available on the physical activity of WA Aboriginal children in remote areas.
A 2018 report (based on the AusPlay survey data from that year) found that Australian children are less likely to participate in organised physical activity outside school hours if:
- they come from a low-income family
- they live in a remote or regional area
- a parent speaks a Language Other Than English (LOTE) at home
- they have three or more siblings.21
The survey also found that only 58 per cent of Australian children and young people from low-income families participate in organised physical activity outside of school compared to 73 per cent of children and young people from middle income families and 84 per cent of children and young people from high income families.22
The WA Government provides financial assistance to encourage WA children and young people to engage in sporting activities through the KidSport program. The program provides up to $150 per year towards fees for approved sporting clubs for children and young people aged five to 18 years from low income families.
The 2019–20 Annual Report of the Department of Local Government, Sport and Cultural Industries stated that the KidSport program provided 18,596 vouchers (approx. $2.5m worth) throughout the year, including 2,300 Aboriginal applicants, 1,000 from the CALD community and 1,200 children with a disability.23
The report noted that restrictions on community sport between March and June 2020 due to COVID-19 had impacted the number of vouchers issued, but that they were experiencing a significant increase in the number of applications with the resumption of community sport in early 2020–21.24
No data has been publicly reported on whether eligible children and young people have increased their physical activity as a result of the program.
Endnotes
- WA Department of Sport and Recreation 2015, Brain Boost: how sport and physical activity enhance children’s learning, Centre for Sport and Recreation Research, Curtin University.
- Australian Institute of Health and Welfare (AIHW) 2018, Physical activity across the life stages, Cat No PHE 225, AIHW.
- Department of Health, Guidelines for healthy growth & development for children & young people (5 to 17 years), Australian Government [website].
- Commissioner for Children and Young People WA 2020, Speaking Out Survey: The views of WA children and young people on their wellbeing - a summary report, Commissioner for Children and Young People WA.
- Martin K et al 2008, Move and Munch Final Report: Trends in physical activity, nutrition and body size in Western Australian children and adolescents: the Child and Adolescent Physical Activity and Nutrition Survey (CAPANS), Department of Sports and Recreation, WA Government.
- Telford RM et al 2016, Why Are Girls Less Physically Active than Boys? Findings from the LOOK Longitudinal Study, PloS one, Vol 11 No 3.
- The WA Department of Health’s, Health and Wellbeing Surveillance System is a continuous data collection which was initiated in 2002 to monitor the health status of the general population. In 2019, 546 parents/carers of children aged 0 to 15 years were randomly sampled and completed a computer assisted telephone interview between January and December, reflecting an average participation rate of just over 90 per cent. The sample was then weighted to reflect the WA child population.
- Bauman A et al 2019, Physical activity measures for children and adolescents - recommendations on population surveillance: an evidence check rapid review, Sax Institute, p. 14.
- This data has been sourced from individual annual Health and Wellbeing Surveillance System reports and therefore has not been adjusted for changes in the age and sex structure of the population across these years nor any change in the way the question was asked. No modelling or analysis has been carried out to determine if there is a trend component to the data, therefore any observations made are only descriptive and are not statistical inferences.
- To assess against the physical guideline recommendations and relating factors, the survey considered: number of days the child did physical activity for at least 60 minutes in the week prior to interview; the type and duration of physical activity undertaken for transport to or from school/place of study and other places on each of the seven days prior to interview; the type and duration of organised and non-organised moderate to vigorous physical activities undertaken on each of the seven days prior to interview. This was determined through a discussion with a parent/carer with child involvement where possible. Source: 4363.0.55.001 - Australian Health Survey: Users' Guide, 2011-13 - Child Physical Activity (5 to 17 years).
- In subsequent Australian Health Surveys (and National Health Surveys) the physical activity data has not been collected by this age group and jurisdiction.
- Martin K et al 2008, Move and Munch Final Report: Trends in physical activity, nutrition and body size in Western Australian children and adolescents: the Child and Adolescent Physical Activity and Nutrition Survey (CAPANS), Department of Sports and Recreation, WA Government.
- Telford RM et al 2016, Why Are Girls Less Physically Active than Boys? Findings from the LOOK Longitudinal Study, PloS one, Vol 11 No 3.
- This data has been sourced from individual annual Health and Wellbeing Surveillance System reports and therefore has not been adjusted for changes in the age and sex structure of the population across these years nor any change in the way the question was asked. No modelling or analysis has been carried out to determine if there is a trend component to the data, therefore any observations made are only descriptive and are not statistical inferences.
- This data has been sourced from individual annual Health and Wellbeing Surveillance System reports and therefore has not been adjusted for changes in the age and sex structure of the population across these years nor any change in the way the question was asked. No modelling or analysis has been carried out to determine if there is a trend component to the data, therefore any observations made are only descriptive and are not statistical inferences.
- This study used a mixed methods approach of pedometers and questionnaires to collect data on physical activity.
- Martin K et al 2008, Move and Munch Final Report: Trends in physical activity, nutrition and body size in Western Australian children and adolescents: the Child and Adolescent Physical Activity and Nutrition Survey (CAPANS), Department of Sports and Recreation, WA Government, p. vi.
- Australian Bureau of Statistics, 4727.0.55.004 - Australian Aboriginal and Torres Strait Islander Health Survey: Physical activity, 2012–13, Table 9.3 Whether met physical and screen-based activity recommendations by Indigenous status by selected characteristics, Children aged 5–17 years in non-remote areas (proportion).
- Australian Bureau of Statistics note that testing indicated that the way the guidelines had been developed into a survey instrument for use in non-remote areas did not work well in more remote areas of Australia. As a result, in remote areas, minimal data was collected only for the day prior to the interview for a range of physical activities, with no measurement of the intensity of these activities.
- Australian Bureau of Statistics, 4727.0.55.004 - Australian Aboriginal and Torres Strait Islander Health Survey: Physical activity, 2012–13, Remote areas (5 years and over), Table 18.3 Physical activity and sedentary behaviour by age then sex, Aboriginal and Torres Strait Islander children aged 5-17 years in remote areas (proportion).
- Australian Sports Commission 2018, AusPlay Focus: Children’s Participation in Organised Physical Activity Outside of School Hours, Australian Government, p. 12.
- Australian Sports Commission 2018, AusPlay Focus: Children’s Participation in Organised Physical Activity Outside of School Hours, Australian Government. In this report, low income families were defined as those with gross (before tax) household income of less than $55,000 per annum; middle income families were defined as those with gross (before tax) household income between $55,000 and $174,999 per annum; and high income families are those with gross (before tax) household income of $175,000 or more per annum.
- Department of Local Government, Sport and Cultural Industries 2020, Annual Report: 2019-20, WA Government, p. 95
- Ibid.
Last updated August 2021
Over the past decade, it has been increasingly recognised that while media devices provide significant opportunities for learning and development, high levels of screen-based activities can be detrimental to children’s health and wellbeing.1 A high level of screen time is associated with sedentary behaviour, low quality sleep, obesity and for some eye health issues.2,3,4 Although, evidence is mixed, screen time is also increasingly being linked to mental health issues for young people, including anxiety and depression.5,6
Screen time is therefore important for children’s wellbeing from two perspectives; as a measure of how much time is spent in sedentary activities (not being active) and how much time is spent on interacting and managing social media (if used), which may impact their mental health and self-esteem and disrupt healthy sleep patterns.
The Australian Physical activity and exercise guidelines for children and young people (5 to 17 years) recommend that the use of electronic media for entertainment be limited to a maximum of two hours per day and long periods of sitting should be broken up as often as possible.
The guidelines are principally focused on reducing sedentary behaviour – based on the theory that more hours spent viewing a screen means less physical exercise. Although it should be noted that screen time does not report on overall levels of sedentary behaviour, which can include other activities such as reading, sitting or lying down.7
Children now grow up with screens as an integral part of their education and social development, and as more children have access to mobile devices it is increasingly difficult to measure daily screen time.
Due to this shift, it is more critical to focus on the quality of the content being consumed rather than a simple focus on the number of hours of screen time. It is also essential to ensure children do enough physical activity and get high quality sleep.
In 2019, the Commissioner conducted the Speaking Out Survey (SOS19) which sought the views of a broadly representative sample of 4,912 Year 4 to Year 12 students in WA on factors influencing their wellbeing, including a range of questions on access and use of technology.8
While the survey did not ask about the number of hours of daily usage, it is evident from the data that many children use screens on a daily basis for a range of activities and it is likely many do not meet the guidelines given they use screens for entertainment, socialising, communicating, gaming and for educational purposes.
Overall, 43.0 per cent of students in Year 4 to Year 6 reported they spend time using the internet on a smartphone or computer every day or almost every day when they are not at school. This proportion was significantly lower than the proportion for Year 7 to Year 12 students (86.8%).
|
Male |
Female |
Metropolitan |
Regional |
Remote |
All |
|
|
Every day or almost every day |
45.7 |
40.4 |
44.6 |
39.4 |
34.4 |
43.0 |
|
Once or twice a week |
29.4 |
30.0 |
30.3 |
25.8 |
32.7 |
29.7 |
|
Less than once a week |
10.2 |
12.2 |
10.7 |
12.9 |
13.0 |
11.3 |
|
Hardly ever or never |
13.2 |
14.7 |
12.7 |
19.2 |
15.1 |
14.0 |
|
I don't know |
1.5 |
2.7 |
1.6 |
2.7 |
4.8 |
2.0 |
Source: Commissioner for Children and Young People WA 2020, Speaking Out Survey 2019 Data Tables [unpublished]
A lower proportion of children in remote locations than metropolitan locations spent time every day or almost every day using the internet (34.4% compared to 44.6%).
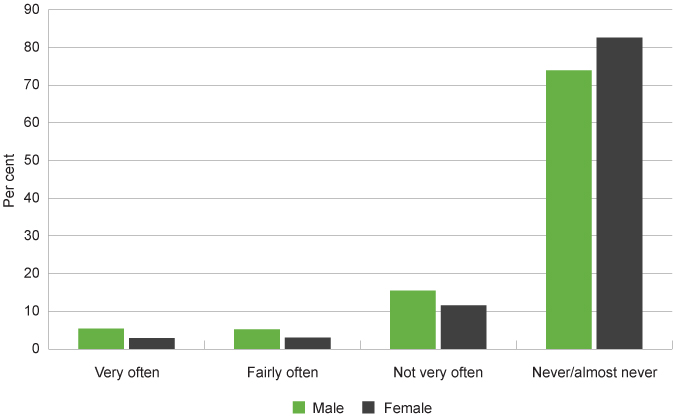
Students in Year 4 to Year 6 were asked how often they go without eating or sleeping because of the internet or electronic games. Most students (78.0%) reported that they never or almost never go without eating or sleeping because of the internet or electronic games. However, a small, but significant minority of students in Year 4 to Year 6 reported that they go without eating or sleeping because of the internet or electronic games very often (4.3%) or fairly often (4.2%).
Students in regional areas were more likely than those in metropolitan and remote areas to report they never or almost never go without eating or sleeping because of the internet or electronic games (84.5% compared to 77.2% and 71.0%, respectively).
|
Male |
Female |
Metropolitan |
Regional |
Remote |
All |
|
|
Very often |
5.4 |
2.9 |
4.6 |
2.4 |
6.3 |
4.3 |
|
Fairly often |
5.2 |
3.0 |
3.9 |
3.7 |
8.9 |
4.2 |
|
Not very often |
15.5 |
11.6 |
14.3 |
9.3 |
13.8 |
13.5 |
|
Never/almost never |
73.9 |
82.6 |
77.2 |
84.5 |
71.0 |
78.0 |
Source: Commissioner for Children and Young People WA 2020, Speaking Out Survey 2019 Data Tables [unpublished]
Female children were significantly more likely than male children to report never or almost never going without eating or sleeping because of the internet or electronic games (female: 82.6%; male: 73.9%).
Proportion of Year 4 to Year 6 students reporting how often they go without eating or sleeping because of the internet or electronic games by gender, per cent, WA, 2019
Source: Commissioner for Children and Young People WA 2020, Speaking Out Survey 2019 Data Tables [unpublished]
In contrast, female students in high school were significantly less likely than male high school students to never or almost never go without eating or sleeping because of their mobile phones (female: 60.9%; male: 70.6%). For more information, refer to the Screen time measure in the Physical health indicator for the 12 to 17 years age group.
Further analysis of the SOS19 data shows that there is a significant association between children not eating or sleeping because of the internet or electronic games and having low self-esteem (not feeling happy with themselves).9
The WA Department of Health administers the WA Health and Wellbeing Surveillance System to monitor the health of WA’s general population, interviewing WA parents and carers about the health of their children aged 0 to 15 years.10 In this survey they ask parents and carers about their children’s screen-based activities and based on these responses reported that the majority (78.6%) of WA children and young people aged five to 15 years met the guidelines in 2019. The data is not disaggregated further by age and therefore we have not reproduced it here.
The last Australian Bureau of Statistics survey with data on children’s screen time was the Australian Health Survey: Physical Activity: 2011–2012. In this survey the average time Australian five to eight year-old children spent on sedentary screen-based activities per day was 98 minutes, while nine to 11 year-old Australian children spent 119 minutes per day.11 These average times are just below the recommended maximum of two hours (120 minutes) per day. These times are likely to have increased significantly over the past 10 years due to the substantial increase in availability and popularity of mobile devices and related applications.
Data from the Longitudinal Study of Australian Children similarly found that children aged six to seven years spent 94 minutes per day on screen-based activities on average. Television was the main medium for screen-based activities for all age groups, with children aged six to seven years watching an average of 80 minutes of television per weekday.12
In this research, the proportion of children who met the screen-based activity guidelines was similar among male and female children. However, there were gender differences in the types of activities. Male children were significantly more likely than female children to spend at least an hour per day on electronic games.13
The findings from this research also suggest that children and young people who enjoy doing physical activities spend less time in front of screens.14 This highlights the importance of engaging children and young people in fun physical activities to provide the foundation for an active life.
In 2020, the Australian Communications and Media Authority published the Kids and mobiles – How Australian children are using mobile phones report which looked at mobile phone ownership and usage amongst Australian children and young people.15 This survey is conducted annually by Roy Morgan and involves interviewing approximately 2,500 children and young people.16
In 2020, the survey found that almost half (46.3%) of children aged six to 13 years used a mobile phone (increased from 41.0% in 2015), with around a third (33%) owning their own mobile phone.17
Mobile phone usage increases as children age with one-quarter (25.0%) of children aged six to seven years having access to a mobile phone and over 80 per cent (81.6%) of 12 to 13 year-olds using a mobile phone. Since 2015, mobile phone usage amongst children has markedly increased across all age groups, except children aged 10 to 11 years.
|
6 to 7 years |
8 to 9 years |
10 to 11 years |
12 to 13 years |
All |
|
|
2015 |
20.2 |
25.2 |
45.6 |
71.6 |
41.0 |
|
2016 |
19.8 |
27.6 |
40.6 |
73.6 |
40.8 |
|
2017 |
23.3 |
30.3 |
44.9 |
79.2 |
44.8 |
|
2018 |
22.4 |
34.9 |
49.2 |
79.4 |
46.9 |
|
2019 |
21.1 |
32.0 |
51.0 |
80.7 |
46.6 |
|
2020 |
25.0 |
30.7 |
46.5 |
81.6 |
46.3 |
Source: Australian Communications and Media Authority (ACMA) 2020, Kids and mobiles: how Australian children are using mobile phones – accessibility data file
This survey also asked children about whether they owned the mobile phone they used. In 2020, one-third (32.6%) of children aged six to 13 years owned their own mobile phone. This includes three-quarters (75.6%) of 12 to 13 year-olds and one-third (32.6%) of 10 to 11 year-olds and 15 per cent of eight to nine year-olds.
|
6 to 7 years |
8 to 9 years |
10 to 11 years |
12 to 13 years |
All |
|
|
2015 |
3.0 |
7.7 |
28.4 |
65.1 |
26.5 |
|
2016 |
2.3 |
10.7 |
26.6 |
66.3 |
27.0 |
|
2017 |
5.0 |
11.5 |
31.5 |
73.0 |
30.8 |
|
2018 |
3.9 |
12.8 |
31.9 |
72.0 |
30.7 |
|
2019 |
5.1 |
14.2 |
35.6 |
73.9 |
32.7 |
|
2020 |
4.8 |
15.3 |
32.6 |
75.6 |
32.6 |
Source: Australian Communications and Media Authority (ACMA) 2020, Kids and mobiles: how Australian children are using mobile phones – accessibility data file
This data shows that the proportion of eight to nine year-olds owning their own mobile phone has doubled from 7.7 per cent in 2015 to 15.3 per cent in 2020.
Children aged six to 11 years most commonly used a mobile phone for playing games, whereas for 12 to 13 year-olds the most common activity was to send or receive texts.
|
6 to 9 years |
10 to 11 years |
12 to 13 years |
|
|
Play games |
67.6 |
70.5 |
74.5 |
|
Take photos/videos |
56.8 |
66.9 |
80.0 |
|
Use apps |
54.0 |
66.8 |
77.5 |
|
Send or receive texts |
26.2 |
63.8 |
84.8 |
|
Call parents/family |
42.2 |
54.6 |
77.3 |
|
Listen to music |
39.2 |
55.2 |
72.5 |
|
Receive calls from parents/family |
34.6 |
52.2 |
76.7 |
|
Send or receive picture messages |
20.2 |
46.4 |
65.3 |
|
Access the internet |
24.8 |
45.8 |
61.0 |
|
Call my friends |
12.7 |
42.5 |
68.6 |
Source: Australian Communications and Media Authority (ACMA) 2020, Kids and mobiles: how Australian children are using mobile phones – accessibility data file
Aboriginal children
Research suggests that Aboriginal families are generally less likely than non-Aboriginal families to have access to the internet at home.18
The ABS conducted the Australian Aboriginal and Torres Strait Islander Health Survey: Physical activity in 2012–13 and found that 46.5 per cent of WA Aboriginal children and young people aged five to 17 years in non-remote areas met the screen-based activity recommendation on all three days prior to the survey, compared with only 36.4 per cent of WA non-Aboriginal children and young people.19
There is no information available on the proportion of WA Aboriginal children in remote areas meeting the screen-based activity (sedentary behaviour) recommendations.
In SOS19, similar proportions of Aboriginal and non-Aboriginal Year 4 to Year 6 students report using the internet on a smartphone or computer when they are not at school every day (42.9% compared to 43.0%).
|
Aboriginal |
Non-Aboriginal |
|
|
Every day or almost every day |
42.9 |
43.0 |
|
Once or twice a week |
23.8 |
30.1 |
|
Less than once a week |
9.9 |
11.4 |
|
Hardly ever or never |
17.1 |
13.8 |
|
I don't know |
6.3 |
1.7 |
Source: Commissioner for Children and Young People WA 2020, Speaking Out Survey 2019 Data Tables [unpublished]
Due to the increasing accessibility and popularity of mobiles devices and screen-based activities, the impact of increased use on children’s physical and emotional wellbeing is critical to monitor now and into the future.
Endnotes
- Yu M and Baxter J 2016, Australian children’s screen time and participation in extracurricular activities, in The Longitudinal Study of Australian Children Annual Statistical Report 2015, Australian Institute of Family Studies.
- Laurson KR et al 2014, Concurrent associations between physical activity, screen time, and sleep duration with childhood obesity, International Scholarly Research Notices: Obesity, Vol 2014.
- Fuller C et al 2017, Bedtime Use of Technology and Associated Sleep Problems in Children, Global Pediatric Health, Vol 4.
- Stiglic N and Viner RM 2019, Effects of screentime on the health and well-being of children and adolescents: a systematic review of reviews, BMJ Open, Vol 9.
- Khouja J et al 2020, Is screen time associated with anxiety or depression in young people? Results from a UK birth cohort, BMC Public Health, Vol 19, No 82.
- Barthorpe A et al 2020, Is social media screen time really associated with poor adolescent mental health? A time use diary study, Journal of Affective Disorders, Vol 274.
- WA Department of Health 2019, Sedentary behaviour, WA Government, [website].
- Commissioner for Children and Young People WA 2020, Speaking Out Survey: The views of WA children and young people on their wellbeing - a summary report, Commissioner for Children and Young People WA.
- Commissioner for Children and Young People WA 2020, Speaking Out Survey 2019 Data Tables, Commissioner for Children and Young People WA.
- The WA Department of Health’s, Health and Wellbeing Surveillance System is a continuous data collection which was initiated in 2002 to monitor the health status of the general population. In 2017, 780 parents/carers of children aged 0 to 15 years were randomly sampled and completed a computer assisted telephone interview between January and December, reflecting an average participation rate of just over 90 per cent. The sample was then weighted to reflect the WA child population.
- Australian Bureau of Statistics (ABS), 43640 Australian Health Survey - National Nutrition and Physical Activity Survey (NNPAS) 2011–12 – Table 20.1 Average time spent on sedentary screen-based activity, children aged 5–17 years (minutes), ABS.
- Yu M and Baxter J 2016, Australian children’s screen time and participation in extracurricular activities, in The Longitudinal Study of Australian Children Annual Statistical Report 2015, Australian Institute of Family Studies, pp. 102, 106.
- Yu M and Baxter J 2016, Australian children’s screen time and participation in extracurricular activities, in The Longitudinal Study of Australian Children Annual Statistical Report 2015, Australian Institute of Family Studies, p. 114.
- Ibid, p. 119-120.
- Australian Communications and Media Authority (ACMA) 2020, Kids and mobiles: how Australian children are using mobile phones, Australian Government [online].
- Australian Communications and Media Authority (ACMA) 2020, Kids and mobiles: how Australian children are using mobile phones - Methodology, Australian Government.
- Australian Communications and Media Authority (ACMA) 2020, Kids and mobiles: how Australian children are using mobile phones – accessibility data file, Australian Government.
- Radoll P & Hunter B 2017, Dynamics of the digital divide: Working Paper No. 120/2017, Centre for Aboriginal Economic Policy Research, The Australian National University, p. 10.
- Australian Bureau of Statistics (ABS), 4727.0.55.004 - Australian Aboriginal and Torres Strait Islander Health Survey: Physical activity, 2012–13, Table 9.3 Whether met physical and screen-based activity recommendations by Indigenous status by selected characteristics, children aged 5–17 years in non-remote areas (proportion), ABS.
Last updated August 2021
Diet has a strong influence on wellbeing from birth. Children need to have a nutritious and balanced diet to grow and develop in a healthy way, and to reduce the risk of developing chronic diseases later in life. Research has shown that eating a wide variety of nutritious foods and limiting consumption of fatty and sugary foods is critical to healthy development and growth.1
Eating regular meals is important because eating irregularly can increase the risk of developing an eating disorder2 and has been linked with a higher risk of diseases such as high blood pressure, Type 2 diabetes and obesity.3
The Australian Government publishes the Australian Dietary Guidelines to provide guidance on foods, food groups and dietary patterns that protect against chronic disease and provide the nutrients required for optimal health and wellbeing. The guidelines are:
- To achieve and maintain a healthy weight, be physically active and choose amounts of nutritious food and drinks to meet your daily energy needs.
- Enjoy a wide variety of nutritious foods from the five food groups every day.
- Limit intake of foods containing saturated fat, added salt, added sugars and alcohol.
- Encourage, support and promote breastfeeding.
- Care for your food; prepare and store it safely.
In 2019, the Commissioner conducted the Speaking Out Survey (SOS19) which sought the views of a broadly representative sample of 4,912 Year 4 to Year 12 students in WA on factors influencing their wellbeing, including a range of questions on physical health.4
Overall, one-half (50.1%) of Year 4 to Year 6 students reported caring very much about eating healthy food, 38.3 per cent of students reported only caring some, 8.9 per cent caring a little and 2.8 per cent not caring at all.
|
Male |
Female |
Metropolitan |
Regional |
Remote |
All |
|
|
Very much |
47.7 |
51.6 |
48.9 |
53.4 |
54.4 |
50.1 |
|
Some |
40.9 |
36.1 |
39.8 |
35.0 |
30.1 |
38.3 |
|
A little |
7.8 |
10.1 |
8.8 |
7.3 |
12.9 |
8.9 |
|
Not at all |
3.5 |
2.2 |
2.5 |
4.2 |
2.5 |
2.8 |
Source: Commissioner for Children and Young People WA 2020, Speaking Out Survey 2019 Data Tables [unpublished]
There were no significant differences in responses between male and female students or students in different geographical regions. There were also no significant differences between Aboriginal and non-Aboriginal students.5
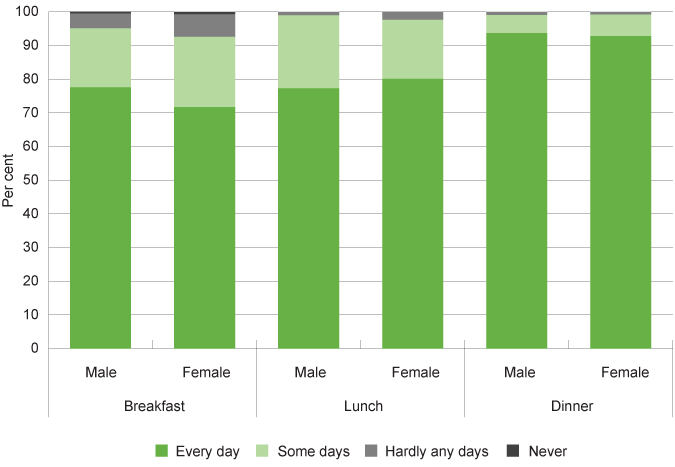
Students in SOS19 were asked how often they usually ate breakfast, lunch and dinner. Across all students in Years 4 to 6, 74.8 per cent reported eating breakfast, 78.4 per cent reported eating lunch and 93.1 per cent reported eating dinner every day.6
Female students in Years 4 to 6 were much less likely than male students to say that they ate breakfast every day (71.7% compared to 77.6% for males). There were no substantial gender differences regarding eating lunch or dinner.
|
Breakfast |
Lunch |
Dinner |
||||
|
Male |
Female |
Male |
Female |
Male |
Female |
|
|
Every day |
77.6 |
71.7 |
77.3 |
80.1 |
93.7 |
92.8 |
|
Some days |
17.5 |
20.9 |
21.4 |
17.4 |
5.2 |
6.1 |
|
Hardly any days |
4.4 |
6.7 |
1.1 |
2.4 |
1.0 |
0.8 |
|
Never |
0.6 |
0.7 |
N/A |
N/A |
N/A |
N/A |
Source: Commissioner for Children and Young People WA 2020, Speaking Out Survey 2019 Data Tables [unpublished]
Proportion of Year 4 to Year 6 students saying they eat breakfast, lunch or dinner every day, some days, hardly any days or never by meal and gender, per cent, WA, 2019
Source: Commissioner for Children and Young People WA 2020, Speaking Out Survey 2019 Data Tables [unpublished]
Notably, across all three regular meal categories, female high school students were less likely than male students to say that they usually ate these meals every day. In particular, female students were significantly less likely than male students to say that they ate breakfast every day, with a majority (61.9%) of female students not eating breakfast every day compared to 41.5 per cent of male students.7 For more information refer to the Healthy diet measure in the age group 12 to 17 years.
Research suggests that adolescents, particularly young females, often worry about their weight and can idealise ultra-thin bodies. This can lead to attempts to control their weight through unhealthy eating behaviours including meal skipping and using extreme diets.8,9 Thus, the proportion of Year 4 to Year 6 female students not eating breakfast every day (29.3%) may be related to these students starting to restrict their eating due to concerns about their weight and body image.
A key component of the guidelines are the recommended daily serves of fruit and vegetables.
|
4 to 8 years |
9 to 11 years |
|
|
Minimum recommended number of serves of vegetables per day |
||
|
Boys |
4½ |
5 |
|
Girls |
4½ |
5 |
|
Minimum recommended number of serves of fruit per day |
||
|
Boys |
1½ |
2 |
|
Girls |
1½ |
2 |
Source: National Health and Medical Research Council 2013, Australian Dietary Guidelines
The guidelines for fruit and vegetable consumption were revised by the National Health and Medical Research Council (NHMRC) in 2013. This had the effect of increasing the recommended serves of vegetables and reducing the recommended amount of fruit for some age groups.10
The WA Department of Health administers the WA Health and Wellbeing Surveillance System to monitor the health of WA’s general population, which includes interviewing WA parents and carers about the health of their children aged 0 to 15 years.11 In this survey they ask parents and carers about their children’s eating behaviours and based on these responses determine the proportion of WA children and young people meeting the fruit and vegetable consumption guidelines.
This survey reports little change in children’s fruit and vegetable consumption since 2014.
A very high proportion (96.0%) of children aged four to eight years of age are meeting the guidelines for fruit consumption. A smaller, but still substantial proportion (61.3%) of children in the older age groups are meeting the requirements for fruit consumption.
|
Consuming recommended serves of fruit |
Consuming recommended serves of vegetables |
|||
|
4 to 8 years |
9 to 15 years |
4 to 8 years |
9 to 15 years |
|
|
2014 |
97.3 |
64.0 |
11.7 |
8.8 |
|
2015 |
99.2 |
62.7 |
24.5 |
6.5 |
|
2016 |
97.8 |
59.6 |
12.4 |
8.3 |
|
2017 |
98.5 |
61.7 |
7.4* |
4.1 |
|
2018 |
96.3 |
65.4 |
17.1 |
6.2* |
|
2019 |
96.0 |
61.3 |
7.8 |
7.6* |
Source: Dombrovskaya M et al 2020, Health and Wellbeing of Children in Western Australia in 2019, Overview and Trends. Department of Health, Western Australia (and previous years’ reports) 12
*Prevalence estimate has a relative standard error of 25 per cent to 50 per cent and should be used with caution.
Note: As the consumption of half serves is not captured in the questions currently asked in the WA Health survey, for the purposes of reporting, the recommended number of serves is rounded down to the nearest whole number.
Only a very small proportion of WA children and young people are meeting the recommended guidelines for vegetable consumption. In both age groups the proportion of children and young people eating sufficient vegetables is very low at less than eight per cent in each case.
The Australian Bureau of Statistics conducted the National Health Survey in 2014–15 and 2017–18 which reported on daily intake of fruit and vegetables for children. This data is relatively consistent with the results of the WA Health and Wellbeing Surveillance System, although the proportion of children meeting the recommended guidelines for fruit consumption are lower.
|
2014-15 |
2017-18 |
||||
|
4 to 8 years |
9 to 11 years |
4 to 8 years |
9 to 11 years |
||
|
Fruit |
WA |
71.9 |
61.1* |
85.1 |
80.2* |
|
Australia |
73.1 |
69.9 |
77.8 |
74.2 |
|
|
Vegetables |
WA |
5.0 |
2.6 |
6.8 |
0.0** |
|
Australia |
3.3 |
3.8 |
3.8 |
5.9 |
|
Source: Australian Bureau of Statistics: National Health Survey: Updated Results, 2014–15 — Australia, Table 17.3 Children's daily intake of fruit and vegetables and main type of milk consumed, Proportion of persons, WA and Australia and National Health Survey: First Results, 2017–18 — Australia, Table 17.3 Children's consumption of fruit, vegetables, selected sugar sweetened and diet drinks, Proportion of persons, WA and Australia
* Proportion has a margin of error >10 percentage points which should be considered when using this information.
** The zero result means there was no data collected for this category in the sample. It does not represent a population estimate.
The ABS also conducted the National Aboriginal and Torres Strait Islander Health Survey in 2018–19.
|
4 to 8 years |
9 to 11 years |
|
|
Adequate daily fruit intake |
69.6 |
61.7 |
|
Adequate daily vegetable intake |
2.4 |
3.9 |
Source: Australian Bureau of Statistics, National Aboriginal and Torres Strait Islander Health Survey, Australia, 2018–19, Table 17.3 Selected dietary indicators, by age, sex and remoteness, Aboriginal and Torres Strait Islander children aged 2–17 years, 2018–19, Proportion of persons
Consistent with the results for all WA children, the majority of Aboriginal children in Australia were not consuming sufficient vegetables in 2018–19.
Fresh fruit and vegetables have less availability and affordability in remote and regional locations, where a large proportion of Aboriginal children and young people live.13 The 2013 WA Food Access and Cost Survey found that food costs increased significantly with distance from Perth, and cost substantially more in very remote areas. At the same time, fruit and vegetable quality was generally lower in remote communities.14
Research also suggests that people living in poverty or with low incomes are more likely to eat calorie rich (high fat, high sugar) foods. The poverty rate for Aboriginal Australians is significantly higher than for non-Aboriginal Australians.15
Refer to the following resource for a more detailed discussion on nutrition among Aboriginal communities:
Lee A and Ride K 2018, Review of nutrition among Aboriginal and Torres Strait Islander people, Australian Indigenous HealthInfoNet.
The low level of vegetable consumption for all WA children is of significant concern.
Guideline three of the Australian Dietary Guidelines also recommends that individuals should limit intake of foods and drinks containing saturated fats and added sugars such as biscuits, cakes, confectionary, sugar-sweetened soft drinks and cordials, fruit drinks and sports drinks.16
Reducing children’s sugar consumption has been highlighted as particularly critical. Sugar consumption in childhood is directly linked to being overweight or obese, and having dental health conditions, both of which impact lifelong health.17 There is also strong evidence to suggest that foods and drinks consumed by children early in life establish their preferences for tastes (e.g. sweetness) later in life.18
Unlike serves of fruit and vegetables, the consumption of sugar is more complex to measure as sugar occurs naturally in many foods. The World Health Organisation recommends reducing the intake of free sugars – which include sugars added to foods by the manufacturer, cook or consumer plus those naturally present in honey, syrups and fruit juices – to less than 10 per cent of total energy intake in both adults and children.19
There is limited data on WA children’s consumption of sugar.
The ABS National Health Survey collects data on children’s consumption of sugar-sweetened drinks based on parent reports.
|
4 to 8 years |
9 to 11 years |
|
|
WA |
67.6 |
64.6* |
|
Australia |
69.4 |
56.3 |
Source: Australian Bureau of Statistics, National Health Survey, First Results 2017–18 – Australia and Western Australia, Table 17.3 Children's consumption of fruit, vegetables, and selected sugar sweetened and diet drinks
* Proportion has a high margin of error and should be used with caution.
Note: Sugar-sweetened drinks includes soft drink, cordials, sports drinks or caffeinated energy drinks. May include soft drinks in ready to drink alcoholic beverages. Excludes fruit juice, flavoured milk, 'sugar free' drinks, or coffee / hot tea.
In the 2017–18 survey they report that 67.6 per cent of WA children aged four to eight years and 64.6 per cent of children aged nine to 11 years were reported by their parents as not usually consuming sugar-sweetened drinks. This was similar to the results for Australia for the 4 to 8 years age group, while, subject to the high margin of error, a higher proportion of WA children aged 9 to 11 than Australian children the same age do not consume sugar-sweetened drinks.
Endnotes
- National Health and Medical Research Council 2013, Australian Dietary Guidelines: Providing the scientific evidence for healthier Australian diets, Canberra, National Health and Medical Research Council.
- O’Connor M et al 2017, Eating problems in mid-adolescence, in The Longitudinal Study of Australian Children Annual Statistical Report 2017, Australian Institute of Family Studies, pp. 113-124.
- Pot G et al 2016, Meal irregularity and cardiometabolic consequences: Results from observational and intervention studies, Proceedings of the Nutrition Society, Vol 75 No 4.
- Commissioner for Children and Young People WA 2020, Speaking Out Survey: The views of WA children and young people on their wellbeing - a summary report, Commissioner for Children and Young People WA.
- Commissioner for Children and Young People WA 2020, Speaking Out Survey 2019 Data Tables, Commissioner for Children and Young People WA.
- Ibid.
- Ibid.
- O’Connor M et al 2017, Eating problems in mid-adolescence, in The Longitudinal Study of Australian Children Annual Statistical Report 2017, Australian Institute of Family Studies, p. 117.
- Aparicio-Martinez P et al 2019, Social Media, Thin-Ideal, Body Dissatisfaction and Disordered Eating Attitudes: An Exploratory Analysis, International Journals of Environmental Research and Public Health, Vol 16.
- Prior to 2013, children aged four to 11 years of age were recommended to eat at least one serve of fruit each day, while 12 to 18 year olds were recommended to eat three serves. While children aged four to seven years of age were recommended to eat at least two serves of vegetables each day, eight to 11 year olds eat at least three serves a day and 12 to 15 year olds eat at least four serves a day. NHMRC, Australian dietary guidelines for children and adolescence 2003 (since rescinded).
- The WA Department of Health’s, Health and Wellbeing Surveillance System is a continuous data collection which was initiated in 2002 to monitor the health status of the general population. In 2017, 780 parents/carers of children aged 0 to 15 years were randomly sampled and completed a computer assisted telephone interview between January and December, reflecting an average participation rate of just over 90 per cent. The sample was then weighted to reflect the WA child population.
- This data has been sourced from individual annual Health and Wellbeing Surveillance System reports and therefore has not been adjusted for changes in the age and sex structure of the population across these years nor any change in the way the question was asked. No modelling or analysis has been carried out to determine if there is a trend component to the data, therefore any observations made are only descriptive and are not statistical inferences.
- Department of the Prime Minister and Cabinet 2015, Aboriginal and Torres Strait Islander Health Performance Framework 2014 Report, 2.19 Dietary behaviours, Australian Government.
- Pollard CM et al 2015, Food Access and Cost Survey 2013 Report, WA Department of Health.
- Davidson P et al 2018, Poverty in Australia, 2018, Australian Council of Social Services (ACOSS), UNSW Poverty and Inequality Partnership Report No 2, ACOSS, p. 65.
- National Health and Medical Research Council 2013, Australian Dietary Guidelines: Providing the scientific evidence for healthier Australian diets, National Health and Medical Research Council.
- Diep H et al 2017, Factors influencing early feeding of foods and drinks containing free sugars—a birth cohort study, International Journal of Environmental Research and Public Health, Vol 14 No 10.
- Ibid.
- World Health Organisation (WHO) 2015, Guideline: Sugars intake for adults and children, WHO.
Last updated August 2021
Being overweight or obese in childhood increases the likelihood of poor physical health in both the short and long term. Being obese increases a child’s risk of a range of conditions such as asthma, Type 2 diabetes1 and cardiovascular conditions.2 In recent years more children are being diagnosed with Type 2 diabetes, when it was previously considered a disease of adulthood.3
Children who are overweight or obese are more likely to be overweight or obese in adulthood.4 Overweight or obese children who continue to be overweight or obese in adulthood face a higher risk of developing coronary heart disease, diabetes, certain cancers, gall bladder disease, osteoarthritis and endocrine disorders.5
Obesity in children is also associated with a number of psychosocial problems, including social isolation, discrimination and low self-esteem.6
While obesity is often the focus of research and data, some children and young people are underweight which can be related to body image issues and eating disorders.
In 2019, the Commissioner conducted the Speaking Out Survey (SOS19) which sought the views of a broadly representative sample of 4,912 Year 4 to Year 12 students in WA on factors influencing their wellbeing, including a range of questions on physical health.7
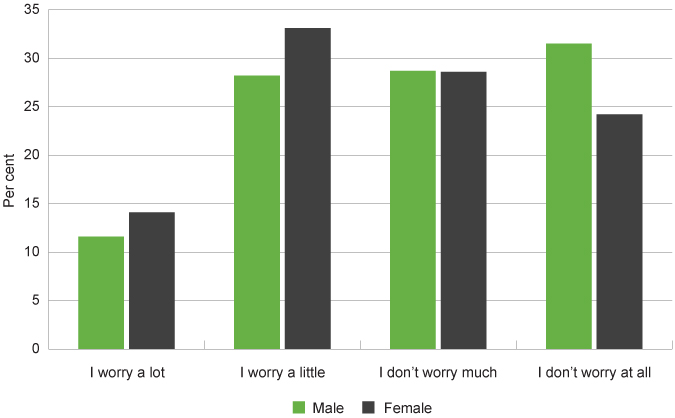
The proportion of male Year 4 to Year 6 students who do not worry at all about their weight at all is significantly higher than that of female students (31.5% compared to 24.2%).
This difference increases as students move through school with the proportion of female students in Years 7 to 12 reporting not worrying at all about their weight falling to 11.7 per cent, while the proportion for male high school students remains relatively unchanged (31.6%).
|
Male |
Female |
Metropolitan |
Regional |
Remote |
All |
|
|
I worry a lot |
11.6 |
14.1 |
13.1 |
11.9 |
13.9 |
13.0 |
|
I worry a little |
28.2 |
33.1 |
31.1 |
29.3 |
30.7 |
30.8 |
|
I don't worry much |
28.7 |
28.6 |
29.2 |
26.4 |
23.8 |
28.3 |
|
I don't worry at all |
31.5 |
24.2 |
26.6 |
32.5 |
31.6 |
28.0 |
Source: Commissioner for Children and Young People WA 2020, Speaking Out Survey 2019 Data Tables [unpublished]
Proportion of Year 4 to Year 6 students reporting they worry a lot, a little, don’t worry much or don’t worry at all about their weight by gender, per cent, WA, 2019
Source: Commissioner for Children and Young People WA 2020, Speaking Out Survey 2019 Data Tables [unpublished]
There were no significant differences in worrying about weight between geographical regions.
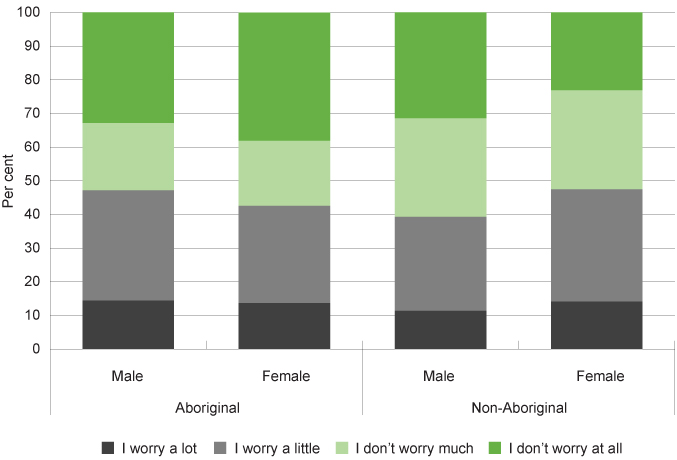
Aboriginal students were more likely than non-Aboriginal students to not worry at all about their weight (35.2% compared to 27.4%). In particular, female Aboriginal students were much more likely than female non-Aboriginal students to not worry about their weight at all (38.2% compared to 23.0%).
|
Aboriginal |
Non-Aboriginal |
|||||
|
Male |
Female |
All |
Male |
Female |
All |
|
|
I worry a lot |
14.4 |
13.7 |
14.0 |
11.4 |
14.1 |
12.9 |
|
I worry a little |
32.8 |
28.9 |
31.2 |
27.9 |
33.4 |
30.8 |
|
I don't worry much |
20.0 |
19.3 |
19.4 |
29.3 |
29.4 |
29.0 |
|
I don't worry at all |
32.9 |
38.2 |
35.3 |
31.5 |
23.0 |
27.4 |
Source: Commissioner for Children and Young People WA 2020, Speaking Out Survey 2019 Data Tables [unpublished]
Proportion of Year 4 to Year 6 students reporting they worry a lot, a little, don’t worry much or don’t worry at all about their weight by Aboriginal status, per cent, WA, 2019
Source: Commissioner for Children and Young People WA 2020, Speaking Out Survey 2019 Data Tables [unpublished]
The WA Department of Health administers the WA Health and Wellbeing Surveillance System to monitor the health of WA’s general population, interviewing WA parents and carers about the health of their children aged 0 to 15 years.8 In this survey parents and carers of children aged five to 15 years are asked to provide their child’s height without shoes and weight without clothes or shoes. A Body Mass Index (BMI) is derived from these figures by dividing weight in kilograms by height in metres squared. BMI scores take into account the age and sex of the young person.9
The use of BMI to measure healthy weight is contested, particularly as it does not distinguish between fat and muscle or the location of the fat.10 BMI is not a diagnostic tool. If a child or young person has a high BMI for their age and sex, they should be referred to a health professional for further assessment considering physical activity and diet, and using other measures such as skin fold thickness or dual energy X-ray absorptiometry (DEXA).11,12,13 BMI is however considered an appropriate tool for population level measurement and trend analysis.14
In 2019, just under one-quarter (22.8%) of WA children and young people aged five to 15 years were categorised as overweight or obese. This proportion has been relatively stable over time, however the past two years have seen successive decreases.
|
Not overweight |
Overweight |
Overweight |
Obese |
|
|
2004 |
73.9 |
26.1 |
19.1 |
7.0* |
|
2005 |
71.7 |
28.4 |
19.5 |
8.9 |
|
2006 |
79.0 |
20.9 |
15.1 |
5.8 |
|
2007 |
82.5 |
17.5 |
12.9 |
4.6* |
|
2008 |
80.3 |
19.7 |
14.0 |
5.7 |
|
2009 |
77.3 |
22.7 |
16.9 |
5.8 |
|
2010 |
77.0 |
23.0 |
17.0 |
6.0 |
|
2011 |
81.2 |
18.7 |
14.5 |
4.2* |
|
2012 |
77.9 |
22.1 |
14.7 |
7.4 |
|
2013 |
78.9 |
21.1 |
15.1 |
6.0 |
|
2014 |
77.4 |
22.6 |
13.9 |
8.7 |
|
2015 |
78.4 |
21.6 |
15.6 |
6.0 |
|
2016 |
76.3 |
23.6 |
18.2 |
5.4 |
|
2017 |
73.7 |
26.3 |
16.4 |
9.9 |
|
2018 |
75.7 |
24.3 |
17.6 |
6.7 |
|
2019 |
77.2 |
22.8 |
14.8 |
8.0 |
Source: Dombrovskaya M et al 2020, Health and Wellbeing of Children in Western Australia in 2019, Overview and Trends. Department of Health, Western Australia (and previous years’ reports)
* Prevalence estimate has a relative standard error of 25 per cent to 50 per cent and should be used with caution.
Note: This is trend data presented by the Department of Health. Data in all years has been standardised by weighting them to the 2011 estimated resident population.
Proportion of children and young people aged 5 to 15 years by BMI categories, per cent, WA, 2004 to 2019
Source: Dombrovskaya M et al 2020, Health and Wellbeing of Children in Western Australia in 2019, Overview and Trends. Department of Health, Western Australia (and previous years’ reports)
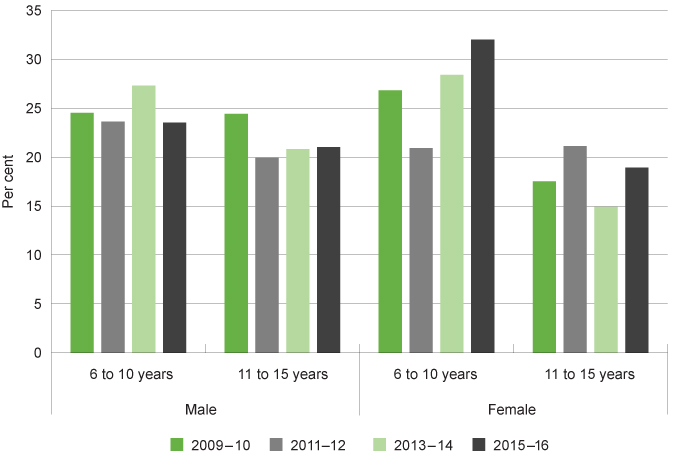
However, age differences exist. In particular, a greater proportion of children aged five to nine years are consistently categorised as obese compared to children and young people aged 10 to 15 years (subject to the margin of error).
|
Overweight |
Obese |
Total |
||||
|
5 to 9 years |
10 to 15 years |
5 to 9 years |
10 to 15 years |
5 to 9 years |
10 to 15 years |
|
|
2012 |
13.5 |
15.5 |
9.4 |
5.9 |
22.9 |
21.4 |
|
2013 |
16.1 |
14.4 |
8.6* |
4.1* |
24.7 |
18.5 |
|
2014 |
15.6 |
12.6 |
15.5 |
3.7* |
31.1 |
16.3 |
|
2015 |
14.9 |
16.2 |
7.8* |
4.6* |
22.7 |
20.8 |
|
2016 |
17.0 |
19.1 |
7.3* |
4.0* |
24.3 |
23.1 |
|
2017 |
16.4 |
16.2 |
14.7 |
6.3* |
31.1 |
22.5 |
|
2018 |
17.9 |
17.2 |
8.5* |
5.2* |
26.4 |
22.4 |
|
2019 |
13.1 |
16.0 |
13.6* |
3.7* |
26.7 |
19.7 |
Source: Dombrovskaya M et al 2020, Health and Wellbeing of Children in Western Australia in 2019, Overview and Trends. Department of Health, Western Australia (and previous years’ reports)
* Prevalence estimate has a relative standard error of 25 per cent to 50 per cent and should be used with caution.
The WA Health and Wellbeing Surveillance System does not report on the proportion of children who are determined to be underweight based on the BMI calculation.
The Australian Bureau of Statistics National Health Survey collects data on BMI categories for children and young people across Australia. The 2017–18 survey provides data for WA, however it has a high margin of error and has not been reproduced here.
Consistent with the WA Department of Health surveillance system, this survey reports that a higher proportion of Australian children aged 8 to 11 years are overweight or obese than young people aged 12 to 15 years.
|
Australia |
|||
|
5 to 7 years |
8 to 11 years |
12 to 15 years |
|
|
Underweight |
7.5 |
9.5 |
7.4 |
|
Normal weight |
65.1 |
65.4 |
71.6 |
|
Overweight |
17.4 |
17.7 |
14.8 |
|
Obese |
10.3 |
6.9 |
6.7 |
|
Overweight/Obese |
27.5 |
25.2 |
20.8 |
Source: Australian Bureau of Statistics, National Health Survey 2017–18, Table 16.3 Children's Body Mass Index, proportion of persons
In the WA Health and Wellbeing survey, over the last six years a higher proportion of female children than male children aged five to 15 years were reported as overweight or obese, however the differences are not statistically significant.15
|
Male |
Female |
|||||
|
Not overweight |
Overweight |
Obese |
Not overweight |
Overweight |
Obese |
|
|
2012 |
76.9 |
14.4 |
8.7 |
78.9 |
15.0 |
6.0 |
|
2013 |
74.8 |
16.6 |
8.7* |
83.0 |
13.7 |
3.3* |
|
2014 |
78.6 |
13.4 |
8.0* |
75.6 |
14.5 |
10.0* |
|
2015 |
78.9 |
14.9 |
6.2* |
77.7 |
16.3 |
5.9* |
|
2016 |
77.8 |
16.5 |
5.7* |
74.9 |
19.8 |
5.3* |
|
2017 |
77.0 |
13.2 |
9.8 |
69.9 |
19.5 |
10.6 |
|
2018 |
81.5 |
12.1 |
6.4* |
69.8 |
23.2 |
7.1* |
|
2019 |
75.0 |
15.9 |
9.0* |
79.5 |
13.3 |
7.2* |
Source: Dombrovskaya M et al 2020, Health and Wellbeing of Children in Western Australia in 2019, Overview and Trends. Department of Health, Western Australia (and previous years’ reports)16
* Prevalence estimate has a relative standard error of 25 per cent to 50 per cent and should be used with caution.
However, when prior year results are disaggregated further by age, it highlights that a much greater proportion of female children aged six to 10 years are reported as overweight or obese (32.0%) than female children aged 11 to 15 years (18.9%).
|
Male |
Female |
|||
|
6 to 10 years |
11 to 15 years |
6 to 10 years |
11 to 15 years |
|
|
2009–2010 |
24.5 |
24.4 |
26.8 |
17.5 |
|
2011–2012 |
23.6 |
19.9 |
20.9 |
21.1 |
|
2013–2014 |
27.3 |
20.8 |
28.4 |
14.9 |
|
2015–2016 |
23.5 |
21.0 |
32.0 |
18.9 |
Source: Custom report provided to the Commissioner for Children and Young People WA from the WA Department of Health Epidemiology Branch, Selected risk factor estimates for WA children using the WA Health and Wellbeing Surveillance System, 2009–2016 [unpublished]
Proportion of young people who are overweight or obese by gender and age group, per cent, WA, 2009–10 to 2015–16 (combined calendar years)
Source: Custom report provided to the Commissioner for Children and Young People WA from the WA Department of Health Epidemiology Branch, Selected risk factor estimates for WA children using the WA Health and Wellbeing Surveillance System, 2009–2016 [unpublished]
These results are consistent with the Australian Bureau of Statistics National Health Survey for 2017–18, which reported that 29.3 per cent of Australian female children aged 5 to 7 years were categorised as overweight and obese compared to 20.0 per cent of female children aged 8 to 11 years.17
Thus, there is a decrease in the prevalence of overweight or obesity for female young people as they move from childhood to adolescence. This pattern is not as evident for male children and young people. These changes for female children and young people could be related to physical changes due to the final growth spurt for females often being between 10 and 12 years18 and possibly the beginning of female young people starting to manage their weight more directly.
The WA survey also asks parents and carers their perception of their child’s weight. For children aged five to 15 years with a BMI that classified them as overweight or obese, the majority (72.9%) had parents/carers who perceived their child’s weight to be normal.19 This highlights that some parents’ and carers’ perceptions of their children’s weight may be overly positive, although in some instances it may indicate how BMI can be an imperfect proxy for unhealthy weight as children age.
In 2020, the Australian Institute of Health and Welfare (AIHW) presented a birth cohort analysis of prevalence of overweight and obesity for a particular group of people born in the same year. They noted that over the last 10 years (2007–08 to 2017–18) there has been no significant change in rates of obesity or overweight in Australian children aged between five and 14 years (23.1% of 5 to 14 year-olds in 2007–08 compared to 24.5% in 2017–18).20
Children and young people living in WA regional and remote locations and areas of greater socio-economic disadvantage are much more likely to be overweight and obese.
|
WA |
Australia |
||
|
Remoteness |
Major cities |
18.5 |
26.2 |
|
Regional and remote |
27.3 |
25.9 |
|
|
Socioeconomic status |
Lowest SES |
27.3 |
33.9 |
|
Highest SES |
15.3 |
22.0 |
|
|
Total |
22.2 |
26.1 |
|
Source: AIHW, Children’s Headline Indicators, Breakdown by population group
Socio-economic disadvantage influences children and young people’s weight for multiple intersecting reasons including limited access to affordable fresh fruit and vegetables and easy access to fast food, availability of primary health services and access to quality outdoor green spaces.21 Additionally, parents with a lower level of education can often have less access to nutritional knowledge which can lead to less healthy dietary practices.22
Aboriginal children and young people
In 2012–13 the Australian Bureau of Statistics conducted the Australian Aboriginal and Torres Strait Islander Health Survey (AATSIHS). In this survey they measured the BMI of participating Aboriginal children and found that Aboriginal children aged five to 10 years were more likely than non-Aboriginal children to be obese (11.2 compared to 7.6%) and less likely to be in the healthy weight range (65.0% compared to 71.7%).23
In 2018–19 the Australian Bureau of Statistics conducted the National Aboriginal and Torres Strait Islander Health Survey which provided data at the jurisdictional level. Results showed the proportion of overweight or obese WA children aged two to 17 to be 35.6 per cent. There was no comparative data for non-Aboriginal WA children in this survey.
A WA study also found that the rates of Type 2 diabetes in WA children and young people increased significantly from 1990 to 2002 and that Aboriginal children and young people were six times more likely to have Type 2 diabetes than the non-Aboriginal population.24
For complex reasons related to colonisation and intergenerational trauma, Aboriginal children are more likely to have a history of poverty, social exclusion, family violence and families with drug and alcohol issues. These factors influence the rate of overweight and obesity in Aboriginal children for a number of reasons. For example, there is evidence that the quality and duration of sleep influences obesity. A recent study concluded that Aboriginal children have a higher BMI than non-Aboriginal children, at least in part, because some Aboriginal children sleep less than non-Aboriginal children.25
Aboriginal adults are 1.6 times more likely to be obese than non-Aboriginal adults, indicating increased risk of developing chronic disease.26 It is therefore critical to reduce the prevalence of overweight and obesity for Aboriginal children by addressing the possible foundational causes.
Endnotes
- Type 2 diabetes is a progressive condition of unknown cause which is associated with modifiable lifestyle risk factors such as obesity. Refer to Diabetes Australia for more information.
- Australian Institute of Health and Welfare (AIHW) 2012, A picture of Australia’s children 2012, Cat No PHE 167, AIHW.
- Davis E 2018, Submission 33 to the Education and Health Standing Committee of the WA Parliament Inquiry: The role of diet in type 2 diabetes prevention and management, Perth Children’s Hospital.
- Venn AJ et al 2007, Overweight and obesity from childhood to adulthood: a follow-up of participants in the 1985 Australian Schools Health and Fitness Survey, The Medical Journal of Australia, Vol 186, No 9.
- Australian Institute of Health and Welfare (AIHW) 2012, A picture of Australia’s children 2012, Cat No PHE 167, AIHW.
- Australian Research Alliance for Children and Youth (ARACY) 2008, ARACY Report Card, Technical Report: The Wellbeing of Young Australians, ARACY.
- Commissioner for Children and Young People WA 2020, Speaking Out Survey: The views of WA children and young people on their wellbeing - a summary report, Commissioner for Children and Young People WA.
- The WA Department of Health’s, Health and Wellbeing Surveillance System is a continuous data collection which was initiated in 2002 to monitor the health status of the general population. In 2017, 780 parents/carers of children aged 0 to 15 years were randomly sampled and completed a computer assisted telephone interview between January and December, reflecting an average participation rate of just over 90 per cent. The sample was then weighted to reflect the WA child population.
- National Health and Medical Research Council 2013, Clinical practice guidelines for the management of overweight and obesity in adults, adolescents and children in Australia, Australian Government, p. 84.
- There is also increasing evidence to suggest that the type of fat is more important than overall weight – for example fat around the stomach has been shown to be more harmful than fat in other locations. Therefore, some research has shown that someone with a relatively high BMI can be healthier than someone with a BMI in the ‘healthy’ range. Refer to Tomiyama et al 2016, Misclassification of cardiometabolic health when using body mass index categories in NHANES 2005-2012, The International Journal of Obesity, Vol 40, No 5.
- Centers for Disease Control and Prevention 2018, About Child and Teen BMI, National Center for Chronic Disease Prevention and Health Promotion (website).
- Nooyens AC 2007, Adolescent skinfold thickness is a better predictor of high body fatness in adults than is body mass index: the Amsterdam Growth and Health Longitudinal Study, The American Journal of Clinical Nutrition, Vol 85, No 6.
- Jensen NSO et al 2016, Review Paper: Comparison of methods to measure body fat in 7-to-10-year-old children: a systematic review, Public Health, Vol 133.
- Centers for Disease Control and Prevention 2018, Body Mass Index: Considerations for practitioners, Department of Health and Human Services USA.
- Merema M and Radomiljac A 2018, Health and Wellbeing of Children in Western Australia in 2017, Overview and Trends, WA Department of Health, p. 35.
- This data has been sourced from individual annual Health and Wellbeing Surveillance System reports and therefore has not been adjusted for changes in the age and sex structure of the population across these years nor any change in the way the question was asked. No modelling or analysis has been carried out to determine if there is a trend component to the data, therefore any observations made are only descriptive and are not statistical inferences.
- Australian Bureau of Statistics, National Health Survey 2017–18, Table 16.3 Children's Body Mass Index, proportion of persons, ABS.
- Zheng W et al 2013, Multilevel Longitudinal Analysis of Sex Differences in Height Gain and Growth Rate Changes in Japanese School-Aged Children, Journal of Epidemiology, Vol 23, No 4.
- Dombrovskaya M et al 2020, Health and Wellbeing of Children in Western Australia in 2019, Overview and Trends. Department of Health, Western Australia.
- Australian Institute of Health and Welfare (AIHW) 2020, Overweight and obesity in Australia: an updated birth cohort analysis, AIHW.
- NSW Council of Social Services (NCOSS) 2016, Overweight and Obesity: Balancing the scales for vulnerable children, NCOSS.
- Ibid.
- Australian Bureau of Statistics (ABS) 2014, Australian Aboriginal and Torres Strait Islander Health Survey: Updated Results, 2012–13 — Australia, Table 9.3 Body Mass Index of children, by age by Indigenous status by sex, proportion of persons, ABS.
- McMahon SK et al 2004, Increase in type 2 diabetes in children and adolescents in Western Australia, Medical Journal of Australia, Vol 180, No 3.
- Deacon-Crouch M et al 2019, The mediating role of sleep in the relationship between Indigenous status and body mass index in Australian school-aged children, Journal of Paediatrics and Child Health, November 2018.
- Department of Prime Minister and Cabinet, Aboriginal and Torres Strait Islander, Health Performance Framework 2014 Report, Australian Government [website].
Last updated August 2021
Long-term health conditions and disability are often inter-related. Long-term health issues and disability can both result in a functional limitation which impacts everyday life for children and young people. People with disability are more likely to develop long-term health conditions, and people with long-term health conditions are more likely to develop disability.1
The most common long-term health issues for children are asthma, diabetes and cancer.2
In 2018, the ABS estimate that 22,400 WA children (11.5%) aged six to 11 years have reported disability.3 In the Disability, Ageing and Carers survey children and young people whose long-term health conditions limit their activities are identified as having disability.4
|
Number |
Per cent |
|
|
Profound or severe core activity limitation (a) |
14,200 |
7.3 |
|
Moderate or mild core activity limitation |
5,200 |
2.7 |
|
Schooling or employment restriction only |
N/A |
N/A |
|
All with specific limitations or restrictions |
20,200 |
10.3 |
|
All with reported disability (b) |
22,400 |
11.5 |
Source: Custom report provided to the Commissioner for Children and Young People WA by the Australian Bureau of Statistics based on the 2018 Disability, Ageing and Carers survey
N/A: Estimate has a relative standard error greater than 50 per cent and is considered too unreliable for general use.
a) Profound or severe core activity limitation comprises:
- profound: the person is unable to do, or always needs help with, a core activity task.
- severe: the person sometimes needs help with a core activity task, and/or has difficulty understanding or being understood by family or friends, or can communicate more easily using sign language or other non-spoken forms of communication.
b) Includes those who do not have a specific restriction or limitation.
The rate of reported disability increases with age, from 4.4 per cent of WA children aged 0 to five years to 11.5 per cent of those aged six to 11 years.5
The types of disability (disability group) that are reported and diagnosed also vary with age. This is in part because as children age, developmental difficulties in certain areas (such as intellectual capacity) become more apparent. Furthermore, there is a lack of formal intellectual testing in very young children.6
In 2018, over two-thirds (67.8%) of Australian young people aged six to 11 years with disability had an intellectual disability and 39.3 per cent had a psychosocial disability, which included a mental health condition or behavioural difficulties.
|
0 to 5 years |
6 to 11 years |
|
|
Sensory or speech |
69.9 |
38.4 |
|
Intellectual |
32.0 |
67.8 |
|
Physical restriction |
23.7 |
20.3 |
|
Psychosocial |
19.7 |
39.3 |
Source: Custom report provided to the Commissioner for Children and Young People WA by the Australian Bureau of Statistics based on the 2018 Disability, Ageing and Carers survey
Note: Children can have one or more types of disability.
Male and female children with disability aged six to 11 years have similar types of disability.
|
Male |
Female |
Total |
|
|
Sensory or speech |
39.9 |
33.6 |
38.4 |
|
Intellectual* |
69.3 |
65.9 |
67.8 |
|
Physical restriction |
19.6 |
23.0 |
20.3 |
|
Psychosocial** |
41.4 |
37.7 |
39.3 |
|
Head injury, stroke, or acquired brain injury |
3.1 |
2.4 |
2.7 |
|
Other |
19.6 |
24.5 |
20.9 |
Source: Australian Bureau of Statistics, Disability, Ageing and Carers, Australia, 2018: Western Australia, Table 3.1: Children aged 0-14 years with disability, living in households, Disability group by Sex and Age – 2018
Note: Children and young people can have one or more types of disability.
* Intellectual disability is when a parent responds that a child/young person has difficulty learning or understanding things.
** Psychosocial disability includes mental illness or a condition requiring help or supervision and social or behavioural difficulties that restrict everyday activities.
Long-term health conditions also have a significant impact on children and young people with disability including impacting everyday activities. In 2018, three-quarters (74.0%) of children and young people aged 0 to 14 years with disability also reported a long-term health condition.7
The most-commonly reported long-term health conditions for Australian children and young people with disability aged 0 to 14 years were autism and related disorders (26.8% of children and young people with disability in 2018), while asthma was also common (16.5%).8
The diagnosis of autism and related disorders in children and young people with disability has increased since 2003 (2003: 6.2%, 2009: 13.0%, 2012: 19.9%, 2015: 24.4%, 2018: 26.8%).9
The diagnosis of phobic and anxiety-related disorders has increased substantially since 2012 (2012: 3.1%, 2015: 9.4%, 2018: 13.7%).
|
2012 |
2015 |
2018 |
|
|
Autism and related disorders |
19.9 |
24.4 |
26.8 |
|
Phobic and anxiety disorders |
3.1 |
9.4 |
13.7 |
|
Other developmental/learning disorders |
9.1 |
14.5 |
14.0 |
|
Attention defecit disorder/hyperactivity |
8.2 |
12.5 |
15.0 |
|
Asthma |
6.3 |
18.3 |
16.5 |
Source: Australian Bureau of Statistics, Disability, Ageing and Carers, Australia, 2018: Table 4.3: Children aged 0-14 years with disability, living in households, Long-term health condition by Sex - 2012, 2015, 2018, Proportion of persons
It should be noted that an increase in reported diagnoses over time does not necessarily represent an increase in the proportion of children and young people with a particular condition – the increase could be due to better diagnostic tools and/or greater community awareness leading to more assessments being carried out.
Diagnosis of many common conditions has been increasing in recent years for both male and female children and young people with disability.
In particular, phobic and anxiety-related disorders have increased from 1.9 per cent of female children and young people with disability in 2012 to 19.5 per cent of female children and young people with disability in 2018.
|
Male |
Female |
|||||
|
2012 |
2015 |
2018 |
2012 |
2015 |
2018 |
|
|
Autism and related disorders |
24.8 |
29.0 |
32.5 |
12.2 |
15.3 |
16.7 |
|
Phobic and anxiety disorders |
3.5 |
8.5 |
10.6 |
1.9 |
9.4 |
19.5 |
|
Other developmental/learning disorders |
9.4 |
15.5 |
13.5 |
6.9 |
14.3 |
15.5 |
|
Attention deficit disorder/hyperactivity |
9.7 |
15.4 |
18.6 |
6.4 |
6.8 |
8.9 |
|
Asthma |
4.3 |
19.9 |
15.9 |
7.3 |
14.8 |
17.2 |
Source: Australian Bureau of Statistics, Disability, Ageing and Carers, Australia, 2018: Table 4.3: Children aged 0-14 years with disability, living in households, Long-term health condition by Sex - 2012, 2015, 2018, Proportion of persons (and previous years’ tables)
Proportion of children and young people aged 0 to 14 years with disability who report a long-term health conditions by most common conditions and gender, per cent, Australia, 2012, 2015, 2018
Source: Australian Bureau of Statistics, Disability, Ageing and Carers, Australia, 2018: Table 4.3: Children aged 0-14 years with disability, living in households, Long-term health condition by Sex - 2012, 2015, 2018, Proportion of persons (and previous years’ tables)
Note: Children and young people may have more than one long-term health condition.
Male children and young people are more likely than female children and young people to be diagnosed with autism and ADHD (and related disorders), while female children and young people are more likely to have anxiety-related disorders.
In recent years there has been recognition that the diagnosis of some behavioural conditions, particularly autism and ADHD, can be biased towards symptoms experienced by male children and young people, while female children and young people’s symptoms are not always recognised or identified correctly.10,11,12
The WA Department of Health published the Burden of Disease in Western Australia, 2015 which reported on the leading causes of disease burden in WA children and young people.13 In this collection, asthma, anxiety disorders, depressive disorders and conduct disorders were in the top four causes of disease burden for both male and female children and young people aged five to 14 years.14
One preventable condition that impacts an unknown number of WA children is Fetal Alcohol Spectrum Disorders (FASD) which is a 'hidden' disability, and easily confused with disobedience or conditions such as Attention Deficit Hyperactivity Disorder (ADHD).15 FASD is an umbrella term which covers a range of possible birth defects and/or developmental disabilities that can be caused by exposure to alcohol prior to birth. It has a significant impact on mental health and increases the likelihood of social and emotional behavioural issues throughout life.16,17
The diagnosis of FASD is complex and until 2016 there was not an Australian diagnostic tool for practitioners.18 As such, FASD is a condition that is under-recognised in Australia and often goes undiagnosed.19 In 2016, The Australian Guide to the diagnosis of Fetal Alcohol Spectrum Disorder (FASD) was released which provides health professionals with the tools necessary to diagnose FASD.20
It is generally recognised that many children and young people in out-of-home care and in contact with youth justice services are living with undetected FASD.21 In 2017, a Telethon Kids Institute research team found that 89 per cent (89 young people) of young people in WA’s Banksia Hill Detention Centre had at least one form of severe neurodevelopmental impairment, while 36 per cent (36 young people) were found to have FASD. It is of significant concern that only two of the young people with FASD had been diagnosed prior to participation in the study.22
In the 2019 report, Inquest into the deaths of: Thirteen children and young persons in the Kimberley region, the WA State Coroner noted that a number of the children and young people were likely to have been on the spectrum for FASD, but that none had been formally diagnosed.23
Screening and assessment for FASD should occur as part of the universal child health checks and at key points across a child's life (e.g. Kindergarten, school entry), as well as when a child or young person enters the child protection or justice system. Any diagnosis needs to trigger appropriate referrals and be linked to clear supports and services, as without this, a diagnosis will have limited impact in terms of improving outcomes for children and young people.
There is limited other data on WA children with disability, although the Commissioner’s Speaking Out Survey included 11 per cent of Year 7 to Year 12 students who reported having a long-term disability. Their perspectives on their health are reported in the Young people with disability measure in the 12 to 17 years age group.
Aboriginal children
There is limited robust data on the prevalence of disability among WA Aboriginal children. This is principally due to a lack of adequate sample size for Aboriginal populations in general surveys and these surveys are often not tailored to incorporate Aboriginal cultures and perspectives on health and wellbeing.24
Furthermore, Aboriginal children and young people can be more likely than non-Aboriginal children and young people to be under-diagnosed for disability or long-term health conditions.25,26,27
The Western Australian Aboriginal Child Health Survey (WAACHS) was a comprehensive cross-sectional study of the health and development of a representative random sample of 5,300 Aboriginal and Torres Strait Islander children and young people aged 0 to 17 years living in 2,000 families across WA, including remote areas.28 The study was conducted in 2000–2001 and has not been repeated.
The WAACHS asked questions about restrictions to WA Aboriginal children and young people’s core activities that included self-care, mobility and communication.29 While the data is not recent and the authors recognised limitations, in general the findings suggested that rates of disability among Aboriginal children were similar to those reported in the non-Aboriginal population.30
However, more recent data from the ABS 2015 Survey of Disability, Ageing and Carers reports that Aboriginal children and young people across Australia are more likely to experience disability than non-Aboriginal children and young people.31
|
Aboriginal |
Non-Aboriginal |
|
|
Profound/severe core activity limitation |
5.9 |
3.9 |
|
Moderate/mild core activity limitation |
4.1 |
1.5 |
|
Schooling or employment restriction only |
2.1* |
0.9 |
|
All with specific restrictions |
11.0 |
6.3 |
|
Has disability but no specific restriction |
2.6* |
0.9 |
|
All with reported disability |
13.8 |
7.2 |
|
No reported disability |
86.8 |
92.9 |
|
Total |
100.0 |
100.0 |
Source: Australian Bureau of Statistics, 44300: Survey of Disability Ageing and Carers: Aboriginal and Torres Strait Islander People with Disability, 2015, Table 2.3 All persons living in households, Indigenous Status by Disability Status, Sex and Age – 2015
* Estimate has a relative standard error of 25 per cent to 50 per cent and should be used with caution.
This data is not available for WA and there is no further breakdown by age group.
The 2018 Survey of Disability, Ageing and Carers did not provide data on Aboriginal children.
There are a range of intersecting social factors that may contribute to the potentially higher prevalence of disability in Aboriginal communities. These can include poverty, low birth weight, poor access to quality primary health care and high levels of alcohol consumption by some mothers during pregnancy.32
Furthermore, differences between Aboriginal and non-Aboriginal people’s conceptualisations of disability may impact identification, diagnosis and treatment. In addition, information may not be available in community languages, culturally appropriate services may not be available and Aboriginal families are more likely to mistrust government organisations due to the legacy of the stolen generations.33
Endnotes
- Australian Institute of Health and Welfare (AIHW) 2015, Chronic conditions and disability, AIHW.
- Australian Institute of Health and Welfare (AIHW) 2005, Selected chronic diseases among Australia’s children, AIHW.
- Data is sourced from a custom report provided to the Commissioner for Children and Young People WA by the Australian Bureau of Statistics based on the 2018 Disability, Ageing and Carers survey. The ABS uses the following definition of disability: ‘In the context of health experience, the International Classification of Functioning, Disability and Health (ICFDH) defines disability as an umbrella term for impairments, activity limitations and participation restrictions. In this survey, a person has a disability if they report they have a limitation, restriction or impairment, which has lasted, or is likely to last, for at least six months and restricts everyday activities’. Australian Bureau of Statistics 2019, Disability, Ageing and Carers, Australia, 2018, Glossary.
- Australian Bureau of Statistics (ABS) 2016, Disability, Ageing and Carers, Australia: Summary of Findings 2015, ABS.
- Custom report provided to the Commissioner for Children and Young People WA by the Australian Bureau of Statistics based on the 2018 Disability, Ageing and Carers survey.
- Australian Bureau of Statistics 2013, Australian Social Trends: 2012, Children with a disability, ABS catalogue no. 4102.0, Commonwealth of Australia, p. 3.
- Australian Bureau of Statistics 2020, Disability, Ageing and Carers, Australia: Summary of Findings, 2018: Children with Disability, ABS.
- Ibid.
- Australian Bureau of Statistics 2013, Australian Social Trends: 2012, Children with a disability, ABS catalogue no. 4102.0, Commonwealth of Australia, p. 3-4 and Australian Bureau of Statistics 2020, Disability, Ageing and Carers, Australia: Summary of Findings, 2018: Children with Disability, ABS.
- Young H 2018, Clinical characteristics and problems diagnosing autism spectrum disorder in girls, Archives de Pédiatrie, Vol 25, No 6.
- Nussbaum NL 2012, ADHD and female specific concerns: a review of the literature and clinical implications, Journal of Attention Disorders, Vol 16, No 2.
- Walters A 2018, Girls with ADHD: Underdiagnosed and untreated, The Brown University Child and Adolescent Behavior Letter, Vol 34, No 11.
- Burden of disease measures the gap between current health and ideal health situations in the population. While one disease may be responsible for considerable loss of life due to early death, another may cause significant loss from disability. The total burden, Disability Adjusted Life Years (DALY) combines both premature deaths (YLL) and disability (YLD) into a single measure. WA Department of Health 2012, Overview of Burden of Disease in Western Australia, 2011, WA Government.
- WA Department of Health 2015, Western Australia Burden of Disease Study 2015, Summary Report, Summary Report, p. 9, WA Government.
- McLean S and McDougall S 2014, Fetal alcohol spectrum disorders: Current issues in awareness, prevention and intervention, CFCA Paper No 20, Child Family Community Australia (CFCA).
- Brown J et al 2018, Fetal Alcohol spectrum disorder (FASD): A beginner’s guide for mental health professionals, Journal of Neurological Clinical Neuroscience, Vol 2, No 1.
- Pei J et al 2011, Mental health issues in fetal alcohol spectrum disorder, Journal Of Mental Health, Vol 20, No 5, pp. 438–448.
- Bower C and Elliott EJ 2016, on behalf of the Steering Group 2016, Australian Guide to the diagnosis of Fetal Alcohol Spectrum Disorder (FASD), Telethon Kids Institute and University of Sydney, p. 4.
- Bower C and Elliott EJ 2016, on behalf of the Steering Group, Australian Guide to the diagnosis of Fetal Alcohol Spectrum Disorder (FASD), Telethon Kids Institute and University of Sydney.
- Ibid.
- McLean S and McDougall S 2014, Fetal alcohol spectrum disorders: Current issues in awareness, prevention and intervention, CFCA Paper No 20, Child Family Community Australia (CFCA).
- Bower C et al 2018, Fetal alcohol spectrum disorder and youth justice: a prevalence study amount young people sentenced to detention in Western Australia, BMJ Open, Vol 8, No 2.
- WA State Coroner 2019, Inquest into the deaths of: Thirteen children and young persons in the Kimberley region, Western Australia, WA Government, p. 256.
- Zubrick SR et al 2004, The Western Australian Aboriginal Child Health Survey: The Health of Aboriginal Children and Young People, Telethon Institute for Child Health Research, p.157.
- Bailey B and Arciuli J 2020, Indigenous Australians with autism: A scoping review, autism, Vol 24, No 5.
- Bower C et al 2018, Fetal alcohol spectrum disorder and youth justice: a prevalence study amount young people sentenced to detention in Western Australia, BMJ Open, Vol 8, No 2.
- Di Pietro N and Illes J 2016, Closing Gaps: Strength-Based Approaches to Research with Aboriginal Children with Neurodevelopmental Disorders, Neuroethics, Vol 9.
- Telethon uses the following definition of level of remote isolation (LORI) ‘LORI allows greater discrimination of the circumstances of survey respondents with respect to their isolation from population centres of various sizes and better differentiates between areas and communities that are extremely remote from major metropolitan centres’. Zubrick SR et al 2004, The Western Australian Aboriginal Child Health Survey: The Health of Aboriginal Children and Young People, Telethon Institute for Child Health Research, p.3.
- Zubrick SR et al 2004, The Western Australian Aboriginal Child Health Survey: The Health of Aboriginal Children and Young People, Telethon Institute for Child Health Research, p.157.
- Ibid, p.157.
- To identify whether a child or young person has a particular type of limitation or restriction, the survey collects information on need for assistance, difficulty experienced, and use of aids or equipment to perform selected tasks from the parent/carer (source: ABS - Explanatory Notes).
- Department of Prime Minister and Cabinet 2014, Aboriginal and Torres Strait Islander: Health Performance Framework Report 2014, 1.14 Disability, Australian Government.
- DiGiacomo M et al 2013, Childhood disability in Aboriginal and Torres Strait Islander peoples: a literature review, International Journal for Equity in Health, Vol 12, No 7.
Last updated August 2021
At 30 June 2021 there were approximately 1,906 children aged six to 11 years in out-of-home care in WA, more than half (57.0%) of whom were Aboriginal.1
Children in care have a higher prevalence of chronic and complex physical, neurological and developmental conditions compared to children in the general population.2 It is therefore critical that children in the care of the state are provided with timely and comprehensive assessments of any health issues and services to meet those issues.
It is a requirement of the WA Department of Communities that children in care receive an initial medical examination within 20 days of entering care and then annual health assessments.3
In 2016, the WA Department for Child Protection (now Department of Communities) published the Outcomes Framework for Children in Out-of-Home Care 2015–16 Baseline Indicator Report. The outcomes framework identified two indicators related to reviewing the physical health of children in out-of-home care.
The first indicator was the ‘proportion of children who had an initial medical examination when entering out-of-home care’. In 2015, only 53.1 per cent of children entering out-of-home care had an initial medical examination.4
The second indicator was the ‘proportion of children who had an annual health check of their physical development'. In this report the Department noted that there were limitations in data accuracy which prevented reporting on this indicator in 2015–16, however data would be reported in 2016–17.5 No data has been reported on this indicator as at publication date.
There is no data available on the physical health of WA children in care, including their physical activity levels, diet or weight.
The lack of up-to-date data on the health of children in care and the low proportion of children and young people provided with an initial medical examination in 2015–16 needs to be urgently addressed.
Endnotes
- Department of Communities 2021, Custom report provided by Department of Communities, WA Government [unpublished].
- Nathanson D and Tzioumi D 2007, Health needs of Australian children living in out of home care, Journal of Paediatric Child Health, Vol 43.
- Department of Child Protection and Family Support (Communities), Casework Practice Manual: Health care Planning, WA Government.
- Department for Child Protection and Family Support 2016, Outcomes Framework for Children in Out-of-Home Care 2015–16 Baseline Indicator Report, p. 5.
- Ibid, p. 10.
Last updated August 2021
Physical health is critical for children’s current wellbeing and their future life outcomes. The physical health of children with disability is often viewed through the lens of their disability and other aspects of health can be overlooked.
There is a complex relationship between physical health and disability, however adults with disability are more likely to have long-term chronic health conditions including heart disease, stroke and diabetes.1
Children with disability who are able to participate in physical activities and have healthy diets are more likely to have better health outcomes over the longer term.2,3
The Australian Bureau of Statistics estimates 22,400 WA children (11.5%) aged six to 11 years had reported disability in 2018.4
In 2019, the Commissioner for Children and Young People (the Commissioner) conducted the Speaking Out Survey which sought the views of a broadly representative sample of 4,912 Year 4 to Year 12 students in WA on factors influencing their wellbeing.5 This survey was conducted across mainstream schools in WA; special schools for students with disability were not included in the sample.
In this survey, 315 Year 7 to Year 12 students with a long-term disability answered questions about their wellbeing, including questions on their physical health. For more information on these students’ views refer to the Physical health indicator for the 12 to 17 years age group.
In 2006, the Physical Activity Study of Children and Adolescents with a Disability (PASCAD) was conducted to examine the physical activity of children/adolescents with disability in metropolitan Perth. This study found that the majority of children and young people with disability were not meeting the recommended physical activity guidelines. They also found that children with disability participated in a narrower range of activities with very low participation rate in community-based team/group activities being the most noticeable difference.6
The children and young people in this study identified social barriers as one of the main obstacles to their physical activity. They reported that non-disabled peers and organisations did not know how to include them in physical activities.7
This study has not been repeated.
No other data exists on the physical health of WA children aged six to 11 years with disability.
Endnotes
- Australian Institute of Health and Welfare (AIHW) 2018, Chronic conditions and disability 2015, Cat no CDK 8, AIHW.
- Heller T et al 2011, Physical Activity and Nutrition Health Promotion Interventions: What is Working for People With Intellectual Disabilities?, Intellectual and Developmental Disabilities Vol 49, No 1.
- Australian Institute of Health and Welfare (AIHW) 2018, Chronic conditions and disability 2015, Cat no CDK 8, AIHW, p. 21.
- Data is sourced from a custom report provided to the Commissioner for Children and Young People WA by the Australian Bureau of Statistics based on the 2018 Disability, Ageing and Carers survey. The ABS uses the following definition of disability: ‘In the context of health experience, the International Classification of Functioning, Disability and Health (ICFDH) defines disability as an umbrella term for impairments, activity limitations and participation restrictions. In this survey, a person has a disability if they report they have a limitation, restriction or impairment, which has lasted, or is likely to last, for at least six months and restricts everyday activities’. Australian Bureau of Statistics 2019, Disability, Ageing and Carers, Australia, 2018, Glossary.
- Commissioner for Children and Young People WA 2020, Speaking Out Survey: The views of WA children and young people on their wellbeing - a summary report, Commissioner for Children and Young People WA.
- Packer TL et al 2006, The Physical Activity Study of Children and Adolescents with a Disability, Curtin University of Technology.
- Ibid.
Last updated August 2021
Most children in WA are healthy, however a significant proportion of children are not consistently engaging in healthy activities such as regular physical exercise, eating a healthy diet and limiting their screen time. This increases their risk of health issues during their childhood and into adulthood.
Available data suggests that most WA children aged six to 11 years are not meeting the recommended physical activity guidelines and female children are less likely to meet the physical activity recommendations than their male peers. Additionally, only a very small proportion (less than 10%) of WA children aged four to 15 years are meeting the recommended guidelines for vegetable consumption. At the same time, while there is limited data on sugar consumption in this age group, it is important to reduce the amount of sugar in all children’s diets.
Many of the children and young people who have participated in the Commissioner’s consultations identified sport and exercise as very important to their wellbeing. They also discussed some of the barriers to getting involved in sporting activities that happened outside of school, including transportation, financial costs, inadequate facilities and equipment, a lack of role models, geographic isolation, parental restrictions and study.1
For a variety of reasons, including socio-economic disadvantage, Aboriginal children are at greater risk of having physical health problems, including obesity, over their lifetime, which contributes to a higher risk of chronic disease. Life expectancy is 8.6 years lower for Aboriginal men, and 7.8 years lower for Aboriginal women than non-Aboriginal WA adults.2 The difference in life expectancy is largely due to a higher incidence of chronic diseases, including heart disease, diabetes and various cancers.3
Socio-economic disadvantage, including parental income levels, education and access to health services have a significant influence on health in childhood.4 The data supports this, as Aboriginal people living in the most disadvantaged areas - a higher proportion of whom are living in remote areas - have the lowest life expectancy.5
The WA Department of Health’s strategy to improve health outcomes for Aboriginal children is encompassed in its WA Aboriginal Health and Wellbeing Framework 2015–2030.
Improving the physical health of children in WA will require multifaceted interventions where evidence-based community level programs are combined with population-level strategies. Some key policy strategies include:6
- policies and programs which improve and promote access to recreational physical activity, including the creation of more community-based environments that provide space for accessible recreational activity and safe unstructured outdoor play and improved transport options, such as bike paths
- supporting all children and their parents, including those with disability and living in regional or remote areas, to participate in playgroups, organised sport and other recreational activities
- policies and programs to ensure all children and young people have access to an adequate and sustainable supply of affordable, healthy, nutritious food
- limiting the availability and appeal of unhealthy food and beverages through marketing regulations and taxation policies
- programs and policies, including education and information campaigns to inform and support parents and carers to maximise health, physical activity, good nutrition and limiting screen time for children
- health advice and preventative services delivered to parents in primary healthcare settings
- programs, guidelines and infrastructure to enable schools to support regular physical activity and healthy eating
- broad strategies that address the social determinants of health including poverty and disadvantage.
Where possible, it is also important for the home environment to be supportive of outdoor play. Recent research in WA has shown that the main factor associated with increased playtime for children was the number of fixed play structures (such as, sandpits, swings etc.) at home, with each additional piece of equipment adding an average of five minutes to a child’s daily playtime.7 When outdoor play at home is restricted, community parks with play equipment are essential.
While data shows rates of being overweight and obese are increasing for some age groups, there is also considerable pressure to strive for unattainable and unrealistic body images which can encourage body dissatisfaction and unhealthy eating behaviours.8
Problematic eating behaviours such as restrictive dieting and skipping meals increase the risk of developing an eating disorder which can have long-term health impacts. It is important to encourage and promote healthy eating and nutrition during childhood to reduce the potential for these behaviours to occur later in life.9
Policies that aim to address rates of overweight and obese children must be formulated in ways that are sensitive and safe and give serious consideration to potentially harmful impacts on future self-esteem and body image.10,11
Data gaps
More information is needed on the prevalence of FASD in Australia and greater awareness and knowledge of FASD in healthcare and family services is necessary to ensure children are properly diagnosed and receive services and support as early as possible.
There is limited data on WA Aboriginal children’s physical health. In 2001 and 2002 the Telethon Institute for Child Health Research (now Telethon Kids Institute) conducted the Western Australian Aboriginal Child Health Survey. Telethon Kids Institute are undertaking a follow-up project to this survey which will analyse outcomes for the children and families surveyed.
The Australian Bureau of Statistics conducted the National Aboriginal and Torres Strait Islander nutrition and physical activity survey (NATSINPAS) in 2011–2013. This survey provided limited data broken down by Australian jurisdiction and also not been repeated since that time. The Commissioner’s Speaking Out Survey provides some current insights into Aboriginal children and young people’s health, however more targeted research is needed.
The lack of data on WA Aboriginal children’s health is a significant gap considering the poorer health outcomes experienced by Aboriginal peoples compared to non-Aboriginal peoples.12
The limited data being collected and reported on the physical health of WA children in out-of-home care is of concern. That only 53.1 per cent of children entering out-of-home care had an initial medical examination in 2015 is of significant concern. The lack of publicly available data makes it difficult to assess whether this issue has been remediated.
There is very limited data available on the health of children with disability. The Australian Bureau of Statistics Disability, Ageing and Carers survey is conducted every three years, however does not always provide detailed data on children and young people in WA.
Endnotes
- Commissioner for Children and Young People 2018, Policy Brief March 2018: Recreation, Commissioner for Children and Young People WA.
- Australian Bureau of Statistics 2018, Life Tables for Aboriginal and Torres Strait Islander Australians, ABS.
- Australian Institute of Health and Welfare (AIHW) 2010, Contribution of chronic disease to the gap in adult mortality between Aboriginal and Torres Strait Islander and other Australians, Cat No IHW 48, AIHW.
- Australian Institute of Health and Welfare (AIHW) 2017, Australia’s Health 2016: 4.2 Social determinants of Indigenous health, AIHW.
- Australian Bureau of Statistics (ABS) 2018, Life Tables for Aboriginal and Torres Strait Islander Australians, 2015-2017, ABS.
- For more information refer: Preventative Health Taskforce 2008, Australia: The Healthiest Country by 2020: A discussion paper prepared by the National Preventative Health Taskforce and Public Health Advocacy Institute of WA, Obesity [website].
- Armstrong G 2019, Associations between the home yard and preschoolers’ outdoor play and physical activity, Public Health Research & Practice, Vol 29, No 1.
- O’Connor M et al 2017, Eating problems in mid-adolescence, in The Longitudinal Study of Australian Children Annual Statistical Report 2017, Australian Institute of Family Studies, p. 113.
- Ibid, p. 113.
- Russell-Mayhew S 2012, Mental Health, Wellness, and Childhood Overweight/Obesity, Journal of Obesity, Vol 2012.
- O’Dea JA 2012, Studies of obesity, body image and related health issues among Australian adolescents: how can programs in schools interact with and complement each other?, Journal of Student Wellbeing, Vol 4 No 2.
- Australian Institute of Health and Welfare (AIHW) 2015, The health and welfare of Australia’s Aboriginal and Torres Strait Islander peoples: 2015 – Health and disability key points [website].
For further information on physical health for young children refer to the following resources:
- Active Healthy Kids Australia 2018, Muscular Fitness: It’s Time for a Jump Start. The 2018 Active Healthy Kids Australia Report Card on Physical Activity for Children and Young People, Active Healthy Kids Australia.
- Australian Institute of Health and Welfare 2018, Physical activity across the life stages, Cat no PHE 225, AIHW.
- Child and Adolescent Health Services, Community Health Manual Guideline: Overweight and Obesity, WA Government.
- Commissioner for Children and Young People 2014, Policy Brief November 2014: Obesity, Commissioner for Children and Young People WA.
- Commissioner for Children and Young People 2018, Policy Brief March 2018: Recreation, Commissioner for Children and Young People WA.
- Lee A and Ride K 2018, Review of nutrition among Aboriginal and Torres Strait Islander people, Australian Indigenous HealthInfoNet.
- National Health and Medical Research Council 2013, Australian Dietary Guidelines: Providing the scientific evidence for healthier Australian diets, Canberra, National Health and Medical Research Council.
- WA Department of Sport and Recreation 2015, Brain Boost: how sport and physical activity enhance children’s learning, Centre for Sport and Recreation Research, Curtin University.