Risk-taking and healthy behaviours
Most young people in WA engage in healthy behaviours, yet participating in risk-taking behaviour including experimentation with substances and sexual activity can be part of the transition to adulthood. Evidence suggests that the earlier young people commence consuming alcohol and other drugs, the greater the likelihood of dependency and associated problems in later life.1 Good sexual health is also important for young people’s physical health and overall wellbeing and it is critical that young people are well informed and supported to make healthy choices.2
It is imperative to address any health concerns or risky behaviours early to improve future health and wellbeing outcomes and quality of life for young people.3
Last updated August 2021
Some data is available on WA young people aged 12 to 17 years engaging in unhealthy and risk-taking behaviours.
Overview
This indicator considers some key measures of unhealthy and risk-taking behaviours of young people, which include the consumption of alcohol and other drugs, and engagement in unsafe sexual activities.
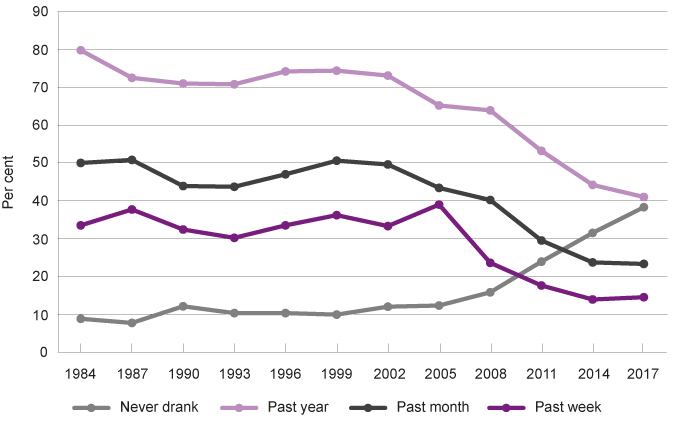
The rates of alcohol use in young people aged 12 to 17 years have declined steadily over the past thirty years in WA. Furthermore, the number of young people in WA who have never consumed alcohol has increased from just under one in ten (9%) in 1984 to three in five (38.3%) young people in 2017.
Prevalence and recency of alcohol use for students aged 12 to 17 years, per cent, WA, 1984 to 2017
Source: Mental Health Commission National Drug Strategy, 2017 ASSAD Alcohol Bulletin, WA Government
Research indicates that there has been a significant decrease in both Aboriginal and non-Aboriginal young people smoking tobacco in the last decade.
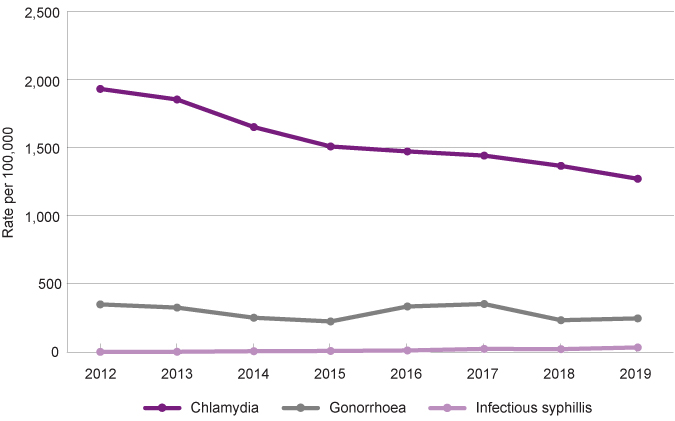
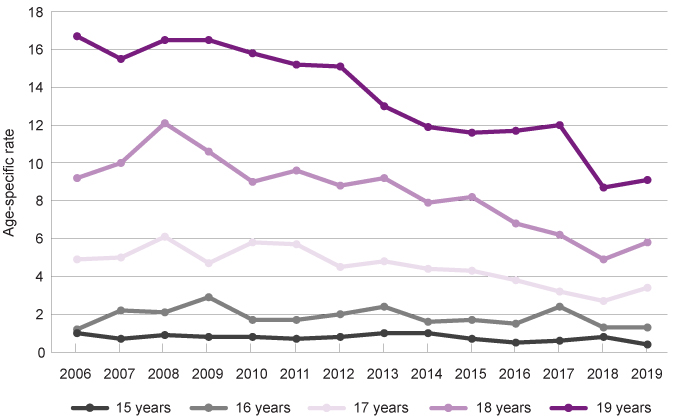
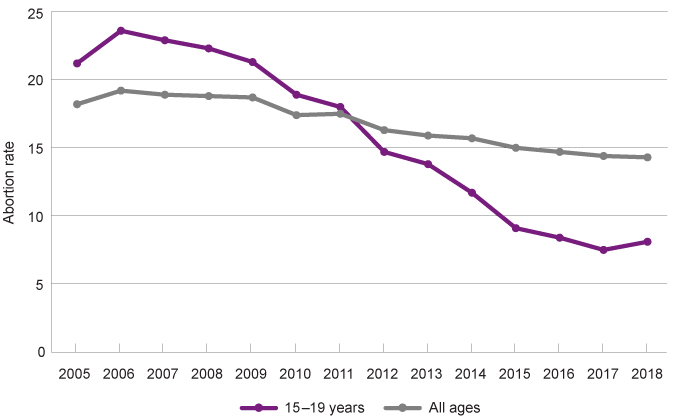
Birth rates for Aboriginal and non-Aboriginal young mothers aged 15 to 19 years in WA have been decreasing over the last 20 years.
Areas of concern
More than one-half (58.1%) of young people in Years 10 to 12 report having drunk more than a few sips of alcohol compared to 20.7 per cent in Years 7 to 9.
While overall trends highlight that illicit drug use is declining, almost one in five (18.1%) young people in WA reported having ever used an illicit drug in 2017.
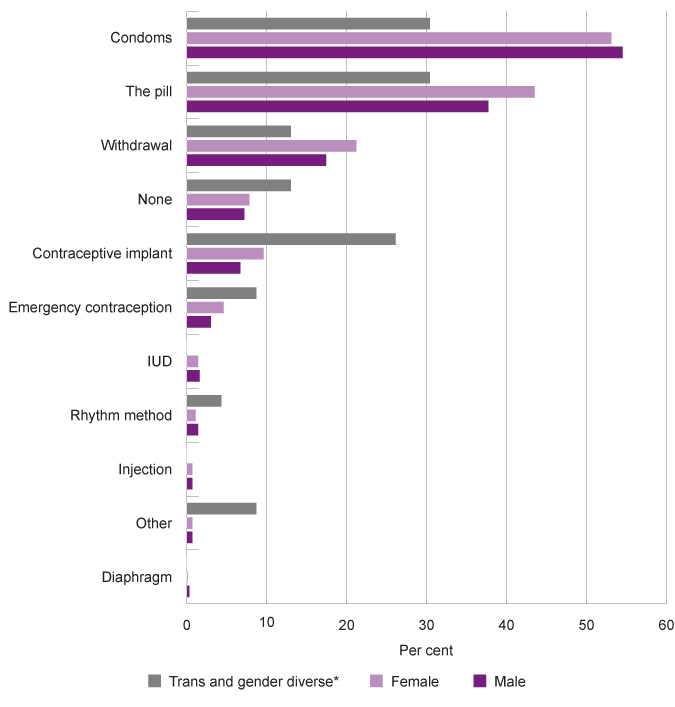
A majority (61.6%) of sexually active Australian young people do not always use a condom during sex and are at risk of contracting a sexually transmissible infection.
Last updated August 2021
Research indicates alcohol can adversely affect brain development in adolescents and be linked to health complications and alcohol-related complications later in life.1 Chronic health conditions linked to alcohol include heart problems, cancer and liver damage.2 Alcohol is also a contributing factor to the three leading causes of death among adolescents – unintentional injuries, homicide and suicide.3
Young people’s alcohol use is also associated with increased risk-taking behaviour including risky sexual behaviour, sexual coercion, drug use, anti-social behaviour, violence and self-harm.
It is therefore critical to focus on reducing risk factors that contribute to young people drinking, to improve the health and wellbeing outcomes for WA young people.
The National Health and Medical Research Council (NHMRC)’s guidelines specify that the safest option for children and young people under the age of 18 years is to consume no alcohol at all. It specifically states that young people under 15 years are at greatest risk of poor health outcomes from drinking alcohol.4
In 2019, the Commissioner conducted the Speaking Out Survey (SOS19) which sought the views of a broadly representative sample of 4,912 Year 4 to Year 12 students in WA on factors influencing their wellbeing, including a range of questions on healthy behaviours.5
This survey showed that more than one-half (57.8%) of young people in Year 7 to Year 12 reported that they have never drunk more than a few sips of alcohol.
|
Male |
Female |
Metropolitan |
Regional |
Remote |
All |
|
|
No |
59.4 |
56.5 |
60.0 |
47.4 |
54.0 |
57.8 |
|
Yes |
36.5 |
39.8 |
36.3 |
49.0 |
40.6 |
38.3 |
|
Prefer not to say |
4.1 |
3.7 |
3.8 |
3.6 |
5.4 |
3.8 |
Source: Commissioner for Children and Young People WA 2020, Speaking Out Survey 2019 Data Tables [unpublished]
There were no significant differences between male and female students or students in different geographical locations, although a higher proportion of young people in regional locations than metropolitan or remote, reported having ever drunk alcohol (49.0% compared to 36.3% and 40.6%).
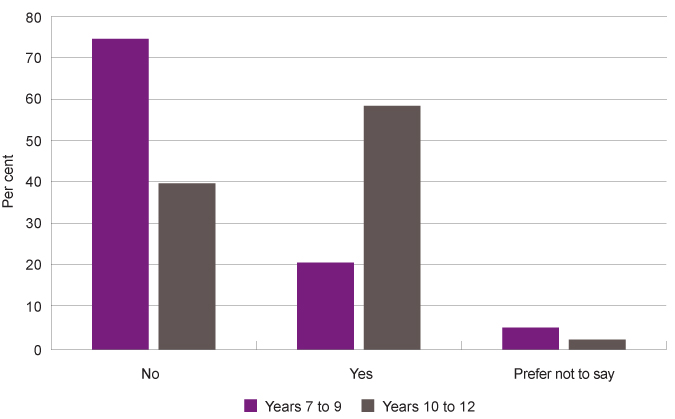
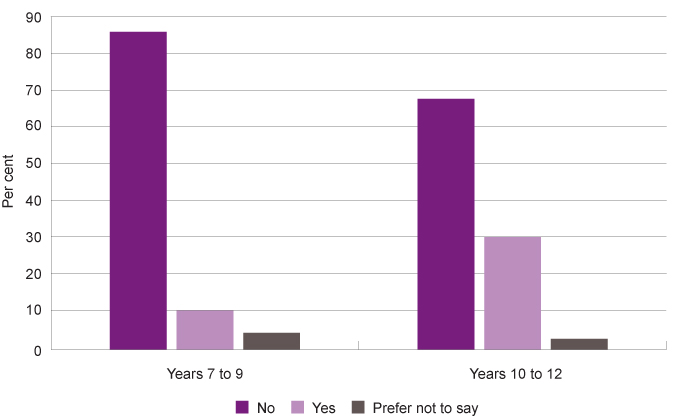
There were significant differences between year groups, with 58.1 per cent of young people in Years 10 to 12 having drunk alcohol compared to 20.7 per cent in Years 7 to 9.
|
Years 7 to 9 |
Years 10 to 12 |
|
|
No |
74.1 |
39.6 |
|
Yes |
20.7 |
58.1 |
|
Prefer not to say |
5.2 |
2.3 |
Source: Commissioner for Children and Young People WA 2020, Speaking Out Survey 2019 Data Tables [unpublished]
Proportion of Year 7 to Year 12 students who reported whether they have ever drunk alcohol (more than just a few sips, like a full can of beer or a glass of wine) by year group, per cent, WA, 2019
Source: Commissioner for Children and Young People WA 2020, Speaking Out Survey 2019 Data Tables [unpublished]
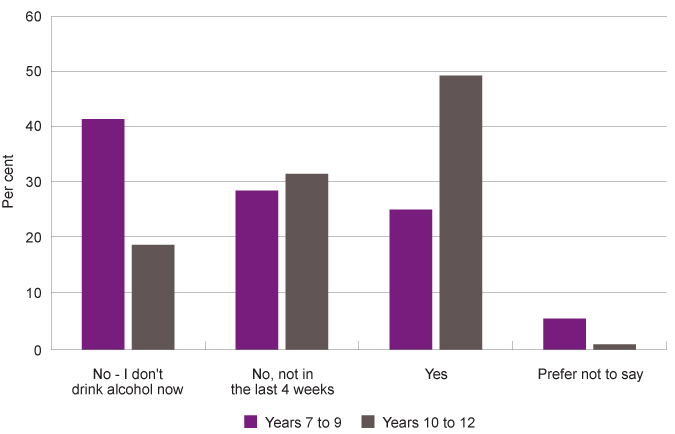
Among those students who had drunk alcohol, 49.0 per cent of Year 10 to 12 and 25.0 per cent of Year 7 to 9 students reported having drunk alcohol in the last four weeks.
|
Years 7 to 9 |
Years 10 to 12 |
|
|
No - I don't drink alcohol now |
41.2 |
18.7 |
|
No, not in the last 4 weeks |
28.4 |
31.4 |
|
Yes |
25.0 |
49.0 |
|
Prefer not to say |
5.5 |
0.9 |
Source: Commissioner for Children and Young People WA 2020, Speaking Out Survey 2019 Data Tables [unpublished]
Proportion of Year 7 to Year 12 students who have ever drunk alcohol responding to the question ‘In the last 4 weeks, did you drink alcohol?’, by response category and year group
Source: Commissioner for Children and Young People WA 2020, Speaking Out Survey 2019 Data Tables [unpublished]
That is, around 28.2 per cent of all Year 10 to 12 students and 5.1 per cent of all Year 7 to Year 9 students reported having drunk alcohol in the last four weeks.
Of the Year 10 to Year 12 students who had drunk alcohol, more than one-in-ten (13.1%) male students had their first drink when they were under 12 years-old compared to 5.9 per cent of female students.
For the students in the survey, 81.2 per cent of students who had drunk alcohol reported they usually drink with friends, 40.2 per cent usually drink with family (which could be siblings) and 17.6 per cent reported they usually drink by themselves. Similar responses were reported by male and female students, across regions and by Aboriginal and non-Aboriginal young people.
The Australian Secondary Students’ Alcohol and Drug (ASSAD) survey is a national survey of young people’s substance use conducted in high schools around Australia every three years. It surveys approximately 20,000 Australian young people aged 12 to 17 years. The most recently published survey was conducted in 2017 with 3,361 WA young people aged from 12 to 17 years from 46 randomly selected government, Catholic and independent schools across the State.
The results for the ASSAD survey differ from the Speaking Out Survey due to different survey methodologies and time periods. In particular, the ASSAD survey defines never drinking as ‘did not even have a sip of an alcoholic drink in their lifetime’.6 Nevertheless, the data provides an analysis of change over time.
According to the ASSAD results, the rates of alcohol use by young people aged 12 to 17 years have declined steadily over the past thirty years in WA.
|
Never drank* |
Past year |
Past month |
Past week |
|
|
1984 |
8.8 |
79.8 |
50.0 |
33.5 |
|
1987 |
7.7 |
72.5 |
50.8 |
37.7 |
|
1990 |
12.1 |
71.0 |
43.9 |
32.4 |
|
1993 |
10.3 |
70.8 |
43.7 |
30.2 |
|
1996 |
10.3 |
74.2 |
47.0 |
33.5 |
|
1999 |
9.9 |
74.4 |
50.6 |
36.2 |
|
2002 |
12.0 |
73.1 |
49.6 |
33.3 |
|
2005 |
12.3 |
65.2 |
43.4 |
39.0 |
|
2008 |
15.8 |
63.9 |
40.2 |
23.6 |
|
2011 |
23.9 |
53.2 |
29.5 |
17.6 |
|
2014 |
31.5 |
44.2 |
23.7 |
13.9 |
|
2017 |
37.8 |
41.8 |
24.1 |
14.7 |
Source: WA Mental Health Commission, 2017 ASSAD Alcohol Bulletin
* Never drank is defined as did not have even a sip of an alcoholic drink in their lifetime.
Prevalence and recency of alcohol use for students aged 12 to 17 years, per cent, WA, 1984 to 2017
Source: WA Mental Health Commission, 2017 ASSAD Alcohol Bulletin
WA high school students who had consumed alcohol in the past week has reduced to 14.7 per cent in 2017 in comparison to 33.5 per cent in 1984. Furthermore, the reported number of high school students in WA that have never consumed alcohol has increased from nine per cent in 1984 to 37.8 per cent in 2017.
These results may reflect strategies that have been developed to reduce alcohol consumption. These strategies include increasing the price of alcohol, limiting physical availability and educating children and young people and their parents and carers on the health and social consequences of alcohol consumption.7,8
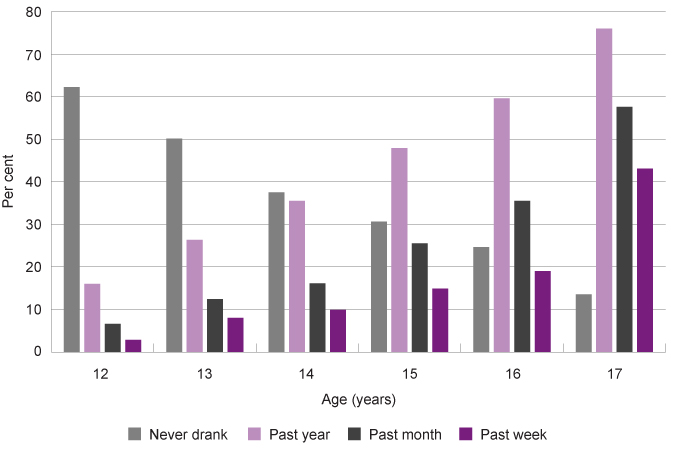
The proportion of young people consuming alcohol increases steadily as they age.
|
12 years |
13 years |
14 years |
15 years |
16 years |
17 years |
|
|
Never drank* |
62.2 |
50.1 |
37.5 |
30.6 |
24.6 |
12.6 |
|
Past year |
16.0 |
26.3 |
35.5 |
47.9 |
59.6 |
77.4 |
|
Past month |
6.6 |
12.4 |
16.1 |
25.5 |
35.5 |
59.8 |
|
Past week |
2.8 |
8.0 |
9.9 |
14.9 |
19.0 |
41.2 |
Source: WA Mental Health Commission, 2017 ASSAD Alcohol Bulletin
* Never drank is defined as did not have even a sip of an alcoholic drink in their lifetime.
Prevalence and recency of alcohol use for students by age, per cent, WA, 2017
Source: WA Mental Health Commission, 2017 ASSAD Alcohol Bulletin
The National Drug Strategy Household Survey (NDSHS) is a triennial survey that collects information on alcohol and drug use patterns, attitudes and behaviours from approximately 24,000 people across Australia.9 The NDSHS asked participants who were 14 to 24 years-old, what age they were when they first drank a standard drink of alcohol. Based on their responses, the average age of first drinking alcohol across Australia was 16.2 years in 2019, up from 16.1 in 2016 and 15.7 in 2013.10
Risky drinking
The NHMRC guidelines do not have risky drinking guidelines for young people, as all alcohol consumption is considered detrimental to their health and wellbeing. However, single occasion risky drinking is believed to be the most common form of risky drinking as most young people do not drink regularly. For adults, risky drinking on a single occasion is defined as five or more standard drinks.11 In general, surveys of young people report against the adult single occasion risky drinking guidelines.
While there has been a welcome increase in the proportion of young people not drinking, the incidence of risky drinking has not changed significantly in the past 20 years. In 1984, 16.1 per cent of WA young people drank at risky levels on a single occasion in the past week, this increased to 27.0 per cent in 1996 and 30.0 per cent in 2017.12
The NDSHS data shows a reduction in single occasion risky drinking from 2010 to 2019 across Australia for young people aged 14 to 17 years (20.5% of young people in 2010 to 8.9% of young people in 2019).13 The data reported by jurisdiction has a very high relative standard error and has not been reproduced here.
The high sampling error across almost all jurisdictions in recent years is of concern, this suggests that the sample sizes were not sufficient to provide valid and reliable estimates for this critical age group by jurisdiction.
The SOS19 data found that of the young people who had drunk in the last four weeks (16.0% of all students), 31.0 per cent had not drunk five or more alcoholic drinks in one session, 44.4 per cent had done so on one occasion in the last four weeks and 14.2 per cent had done so on two or three occasions in the last four weeks. Eight (7.9%) per cent of students who had drunk in the last four weeks reported having had more than four standard drinks on a single occasion on a weekly basis.
While the numbers are small, this equates to about 1.0 per cent of all Year 7 to Year 12 students drinking at risky levels on a weekly basis.
|
Male |
Female |
All |
|
|
None |
34.6 |
28.5 |
31.0 |
|
Once in the past 4 weeks |
42.5 |
46.4 |
44.4 |
|
Two or three times in the past 4 weeks |
12.0 |
15.9 |
14.2 |
|
Every week |
7.7 |
4.0 |
5.5 |
|
Several times a week |
1.9 |
1.8 |
2.4 |
|
Prefer not to say |
N/A |
3.4 |
2.4 |
Source: Commissioner for Children and Young People WA 2020, Speaking Out Survey 2019 Data Tables [unpublished]
Similar proportions of male and female Year 7 to Year 12 students who had drunk alcohol in the last four weeks, had engaged in risky drinking practices.
The NHMRC guidelines state there is a high level of health risk associated with the consumption of any alcohol for ages 15 years and under, therefore many of these WA young people are consuming alcohol at a very risky level.
The Young Australians’ Alcohol Reporting System (YAARS) is a national research project that aimed to provide insight into the risky drinking patterns of Australian young people. In late 2016 and early 2017, a total of 965 14 to 19 year-olds were interviewed or surveyed in WA. From this group, 479 young people were identified as ‘risky drinkers’.14
For these risky drinkers the most popular beverage type was spirits, with 76 per cent of young people drinking spirits at their last risky drinking session. Female young people were more likely to drink spirits (80%) and ready to drink beverages (46%), while male young people were also more likely to drink spirits (71%) followed by beer (67%).15
Parental use of alcohol can have a significant impact on the health and wellbeing of children and young people in their care. For many young people, the family environment is their first introduction to alcohol, with attitudes and behaviours associated with drinking being modelled by carers or parents in the young person’s home. Research has highlighted a parents’ drinking behaviour is positively correlated with adolescents’ use of alcohol.16
In 2011, the Commissioner for Children and Young People consulted with approximately 300 WA young people aged 14 to 17 years about their views on alcohol. More than half of the young people reported that their parents were a significant influence on their decisions about alcohol consumption.17
In the 2017 ASSAD survey, WA young people aged 12 to 17 years who had reported drinking alcohol in the last week also recorded the sources of their alcohol supply. Results highlighted that one in three WA young people sourced their alcohol from their friends (33.6%) and 22.7 per cent sourced it from their parents. A high proportion (15.9%) of 12 to 15 year-olds reported taking alcohol from home without permission.18
Of particular concern is that 24.7 per cent of WA young people aged 12 to 15 years who reported drinking alcohol reported their parents gave it to them.
The Australian Institute of Family Studies conduct the Longitudinal Study of Australian Children and in 2016 explored parental influences on adolescent’s alcohol use. Results indicated a 10 per cent statistically significant increase in drinking levels for young people who had a mother who drank some alcohol and a 5 per cent increase in drinking levels for young people who had a father who drank some alcohol.19
In a two-parent household the prevalence of a young person having consumed alcohol in the last 12 months was approximately 9 per cent where neither parents drank at a risky level,20 16 per cent where the father drank at a risky level and 23 per cent where both parents reported regularly consuming alcohol.21
Aboriginal young people
Both Aboriginal and non-Aboriginal young people in Australia consume alcohol. There are however, significant social factors that increase the risk of alcohol consumption and risky drinking among Aboriginal communities. These intersecting factors include economic marginalisation, discrimination, cultural dispossession, family conflict or violence and family history of alcohol misuse.22
The NDSHS reports a decline in single occasion risky alcohol consumption at least monthly for Aboriginal young people and adults (people aged 14 years and over, including adults) from 2010 (39.4%) to 2019 (35.4%). Furthermore, there was an increase in the proportion of Aboriginal people aged 14 years and over who were drinking at single occasion low risk levels (20.9% in 2010 compared to 27.8% in 2019).23
In 2018–19, the Australian Bureau of Statistics (ABS) conducted the National Aboriginal and Torres Strait Islander Health Survey which included a nationally representative sample of around 13,000 Aboriginal people in remote and non-remote locations. This survey compared alcohol consumption for young people aged 15 to 17 years to the NHMRC guidelines for single occasion risky drinking.
|
2012-13 |
2018-19 |
|
|
Did not exceed NHMRC guidelines |
17.3 |
10.9 |
|
Exceeded NHMRC guidelines |
23.7 |
17.6 |
|
Consumed alcohol 12 or more months ago |
5.7 |
3.4 |
|
Never consumed alcohol |
52.0 |
68.0 |
Source: Australian Bureau of Statistics, Australian Aboriginal and Torres Strait Islander Health Survey, Table 14 Alcohol Consumption – Short term or single occasion risk by age, Indigenous status and sex, 2012-13 – Australia and National Aboriginal and Torres Strait Islander Health Survey, Table 14.3 Alcohol consumption—Single occasion risk by age, sex and Indigenous status, persons aged 15 years and over, 2017–18 and 2018–19
This survey found that there has been a substantial increase in the proportion of Aboriginal young people aged 15 to 17 years who have never consumed alcohol (from 52.0% in 2012–13 to 68.0% in 2018–19).
There is no data available from this survey on alcohol consumption for Aboriginal children and young people in WA.
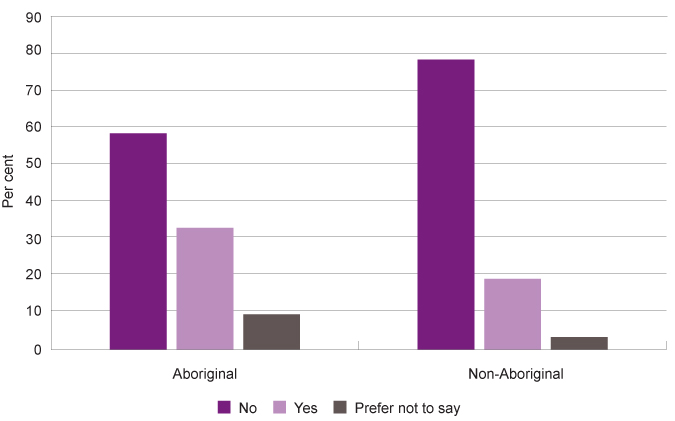
In the SOS19 data, a greater proportion of non-Aboriginal than Aboriginal Year 7 to Year 12 students reported that they have never drunk more than a few sips of alcohol (58.4% compared to 49.9%), although this difference was not statistically significant. A significantly greater proportion of Aboriginal students than non-Aboriginal students reported that they would prefer not to say whether they had drunk alcohol (9.3% compared to 3.5%).
|
Non-Aboriginal |
Aboriginal |
|
|
No |
58.4 |
49.9 |
|
Yes |
38.1 |
40.7 |
|
Prefer not to say |
3.5 |
9.3 |
Source: Commissioner for Children and Young People WA 2020, Speaking Out Survey 2019 Data Tables [unpublished]
Education about alcohol
In SOS19, young people in Years 7 to 12 were asked how much they have learnt about alcohol at school.
Most (77.1%) young people reported that they had learnt a lot (41.1%) or some (36.0%) about alcohol at school. While, 16.3 per cent reported they had only learnt a little bit and 6.7 per cent reported they had learnt nothing.
|
Years 7 to 9 |
Years 10 to 12 |
All |
|
|
Nothing |
9.4 |
3.6 |
6.7 |
|
A little bit |
16.7 |
15.8 |
16.3 |
|
Some |
37.2 |
34.6 |
36.0 |
|
A lot |
36.7 |
46.0 |
41.1 |
Source: Commissioner for Children and Young People WA 2020, Speaking Out Survey 2019 Data Tables [unpublished]
Of concern is that almost one in five (19.4%) students in Years 10 to 12 reported that they had learnt either nothing (3.6%) or a little bit (15.8%) about alcohol in school.
Most (87.9%) high school students reported that they feel like they know enough about the health impacts of alcohol, while 7.1 per cent did not feel like they knew enough and 5.0 per cent were not sure. These proportions were similar for students in Years 7 to 9 and Years 10 to 12.24
Lesbian, gay, bisexual, trans and intersex children
For information on LGBTI young people’s consumption of alcohol, tobacco and other drugs refer to the Measure: Use of illicit drugs.
Culturally and linguistically diverse young people
For information on culturally and linguistically diverse young people’s consumption of alcohol, tobacco and other drugs refer to the Measure: Use of illicit drugs.
Young people in the youth justice system
For information on the consumption of alcohol, tobacco and other drugs of young people in youth detention refer to the Measure: Use of illicit drugs.
Endnotes
-
National Health and Medical Research Council (NHMRC) 2009, Australian guidelines to reduce health risks from drinking alcohol, NHMRC, p. 61.
-
Ibid, p. 120.
-
Australian Drug Foundation (ADF) 2019, Alcohol and young people, ADF.
-
National Health and Medical Research Council (NHMRC) 2009, Australian guidelines to reduce health risks from drinking alcohol, NHMRC, p. 4.
-
Commissioner for Children and Young People WA 2020, Speaking Out Survey: The views of WA children and young people on their wellbeing - a summary report, Commissioner for Children and Young People WA.
-
Guerin N and White V 2018, Statistics and Trends: Australian Secondary School Students’ Use of Tobacco, Alcohol, Over-the-counter Drugs, and Illicit Substances, Centre for Behavioural Research in Cancer Council of Victoria
-
Australian Institute of Health and Welfare (AIHW) 2017, National Drug Strategy Household Survey 2019, Drug Statistics series no 32 Cat no PHE 214, AIHW, p. 26.
-
Department of Health 2017, National Drug Strategy 2017-2026, Australian Government.
-
Australian Institute of Health and Welfare (AIHW) 2017, National Drug Strategy Household Survey 2016: detailed findings, AIHW, p. 3 and 134.
-
Australian Institute of Health and Welfare (AIHW) 2020, Alcohol, tobacco & other drugs in Australia, Table S3.31:Age of initiation, recent drinkers and ex–drinkers aged 14–24, 2001 to 2019 (years), AIHW. This is the average (mean) age that 14–24 year olds first consumed a full serve of alcohol.
-
National Health and Medical Research Council (NHMRC) 2009, Australian guidelines to reduce health risks from drinking alcohol, NHMRC.
-
Mental Health Commission (MHC) 2019, Alcohol trends in Western Australia 2017: Australian school students alcohol and drug survey, MHC.
-
Australian Institute of Health and Welfare 2020, National Drug Strategy Household Survey 2019, Table S.22: People at risk of injury on a single occasion of drinking(a), by age and state/territory, 2007 to 2019 (per cent), AIHW.
-
Pandzic I et al 2017, Young Australians Alcohol Reporting System (YAARS) Report 2016/17 – Western Australian main findings, National Drug Research Institute, Curtin University, p. 7.
-
Ibid, p. 13.
-
Homel J and Warren D 2016, Parental influences on adolescent alcohol use, in The Longitudinal Study of Australian Children Annual Statistical Report 2015, Australian Institute of Family Studies.
-
Commissioner for Children and Young People WA 2011, Speaking out about: Alcohol-related harm on children and young people, Commissioner for Children and Young People WA.
-
Mental Health Commission (MHC) 2019, Alcohol trends in Western Australia 2017: Australian school students alcohol and drug survey, MHC.
-
Homel J and Warren D 2016, Parental influences on adolescent alcohol use, in The Longitudinal Study of Australian Children Annual Statistical Report 2015, Australian Institute of Family Studies, p. 72-73.
-
Risky drinking was categorised as five or more drinks on a single occasion, at least twice a month.
-
Homel J and Warren D 2016, Parental influences on adolescent alcohol use, in The Longitudinal Study of Australian Children Annual Statistical Report 2015, Australian Institute of Family Studies, p. 73.
-
Australian Institute of Health and Welfare (AIHW) 2011, Substance use among Aboriginal and Torres Strait Islander people, AIHW, p. 11.
-
Australian Institute of Health and Welfare (AIHW) 2020, National Drug Strategy Household Survey 2019, , Table 8.2: Use of drugs by Indigenous status, people aged 14 and over, 2010 to 2019 (age standardised col per cent), AIHW.
-
Commissioner for Children and Young People WA 2020, Speaking Out Survey 2019 Data Tables, Commissioner for Children and Young People WA [unpublished].
Last updated August 2021
Smoking greatly increases the risk of many cancers, cardiovascular disease, respiratory diseases and many other serious medical conditions.1 Research has shown that the younger a person starts smoking, the less likely they are to stop.2
In 2019, the Commissioner conducted the Speaking Out Survey (SOS19) which sought the views of a broadly representative sample of 4,912 Year 4 to Year 12 students in WA on factors influencing their wellbeing, including a range of questions on healthy behaviours.3
Overall, more than three-quarters (76.7%) of Year 7 to Year 12 students have never smoked a cigarette, even a few puffs, while 19.6 per cent have tried cigarette smoking.
|
Male |
Female |
Metropolitan |
Regional |
Remote |
All |
|
|
No |
79.2 |
75.1 |
79.1 |
67.7 |
65.2 |
76.7 |
|
Yes |
17.2 |
21.3 |
17.6 |
27.3 |
30.5 |
19.6 |
|
Prefer not to say |
3.6 |
3.6 |
3.5 |
4.9 |
4.3 |
3.6 |
Source: Commissioner for Children and Young People WA 2020, Speaking Out Survey 2019 Data Tables [unpublished]
Of those that have tried cigarette smoking, 59.2 per cent have smoked a whole cigarette. That is, of all high school students, 11.6 per cent have smoked a whole cigarette.
Students in regional and remote locations are more likely to have tried cigarette smoking than those in the metropolitan area (27.3% and 30.5% compared to 17.6%).
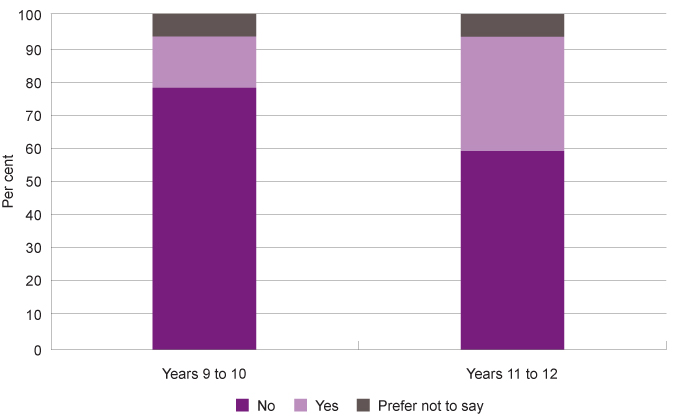
Students in Year 10 to 12 are more likely to have tried cigarette smoking than those in Years 7 to 9 (30.1% compared to 10.4%).
|
Years 7 to 9 |
Years 10 to 12 |
|
|
No |
85.2 |
67.2 |
|
Yes |
10.4 |
30.1 |
|
Prefer not to say |
4.4 |
2.8 |
Source: Commissioner for Children and Young People WA 2020, Speaking Out Survey 2019 Data Tables [unpublished]
Proportion of Year 7 to Year 12 students who reported whether they have ever tried cigarette smoking, even one or two puffs by year group, per cent, WA, 2019
Source: Commissioner for Children and Young People WA 2020, Speaking Out Survey 2019 Data Tables [unpublished]
Most (57.3%) Year 7 to Year 12 students who reported they had tried smoking a cigarette did not smoke now, however one in 10 reported that they now smoke on most days (3.5%) or daily (7.3%).4 This equates to 2.1 per cent of all Year 7 to Year 12 students.
There were no significant differences in cigarette smoking between male and female students in WA.
|
Male |
Female |
All |
|
|
Never, I don't smoke now |
59.7 |
56.8 |
57.3 |
|
Occasionally |
16.0 |
20.0 |
18.2 |
|
Once or twice a month |
5.9 |
4.9 |
5.1 |
|
Once or twice a week |
3.6 |
6.6 |
5.2 |
|
Most days |
4.6 |
1.9 |
3.5 |
|
Daily |
5.7 |
7.9 |
7.3 |
|
Prefer not to say |
4.5 |
1.9 |
3.3 |
Source: Commissioner for Children and Young People WA 2020, Speaking Out Survey 2019 Data Tables [unpublished]
The National Drug Strategy Household Survey (NDSHS) is a triennial survey that in 2019 collected information from approximately 23,000 people across Australia. In this survey participants were asked about their drug use patterns, attitudes and behaviours.
The NDSHS reports on the proportion of people who have ‘never smoked’, however this is actually people who have never smoked more than 100 cigarettes. There is no measure of young people who have never smoked even one puff in the NDSHS.
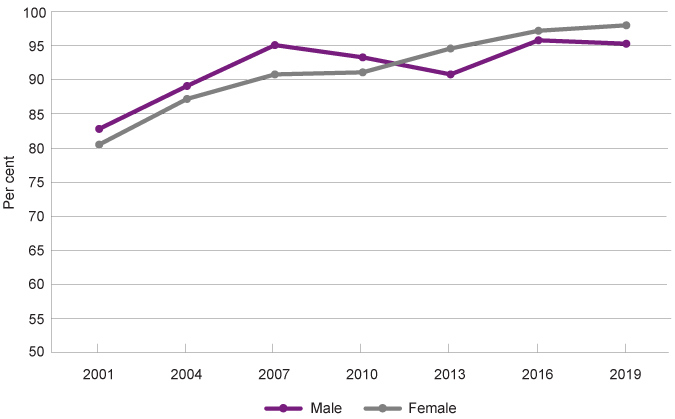
Across Australia, there has been a steady increase in the proportion of young people aged 14 to 17 years who have never smoked more than 100 cigarettes (81.7% in 2001 compared to 96.6% in 2019).
|
Male |
Female |
Total |
|
|
2001 |
82.8 |
80.5 |
81.7 |
|
2004 |
89.1 |
87.2 |
88.1 |
|
2007 |
95.1 |
90.8 |
93.0 |
|
2010 |
93.3 |
91.1 |
92.2 |
|
2013 |
90.8 |
94.6 |
92.6 |
|
2016 |
95.8 |
97.2 |
96.4 |
|
2019 |
95.3 |
98.0 |
96.6 |
Source: Australian Institute of Health and Welfare, National Drug Strategy Household Survey 2019, Table 2.7: Tobacco smoking status, by age and sex, 2001 to 2019
In 2019, female young people across Australia were slightly more likely to have never smoked more than 100 cigarettes in their lifetime than male young people (98.0% compared to 95.3%).
Proportion of young people aged 14 to 17 years who have never smoked (more than 100 cigarettes in their lifetime) by gender, per cent, Australia, 2001 to 2019
Source: Australian Institute of Health and Welfare, National Drug Strategy Household Survey 2019, Table 2.7: Tobacco smoking status, by age and sex, 2001 to 2019
The NDSHS also shows a reduction in Australian young people aged 14 to 19 years smoking on a daily basis from 2010 to 2019 (6.9% of young people in 2010 to 3.7% of young people in 2019).5 Similarly, there has been a concurrent reduction in Australian young people aged 14 to 17 years smoking on a daily basis (subject to the margin of error).
|
14 to 17 years |
14 to 19 years |
|
|
2007 |
4.6 |
7.3 |
|
2010 |
3.7 |
6.9 |
|
2013 |
5.1 |
7.0 |
|
2016 |
2.2* |
3.0 |
|
2019 |
1.9* |
3.7 |
Source: Australian Institute of Health and Welfare, National Drug Strategy Household Survey 2019, Table S.9: Daily tobacco smoking status, by age and state/territory, 2007 to 2019
* Estimate has a relative standard error of 25% to 50% and should be used with caution.
The data reported by jurisdiction has a very high relative standard error and has not been reproduced here.
The high sampling error across almost all jurisdictions in recent years is of concern, this suggests that the sample sizes were not sufficient to provide valid and reliable estimates for this critical age group by jurisdiction.
The Australian Secondary Students’ Alcohol and Drug (ASSAD) survey is a national survey of young people’s alcohol and drug use conducted in high schools around Australia every three years. It surveys approximately 20,000 young people aged 12 to 17 years.
According to results from the 2017 ASSAD survey, 83.0 per cent of Australian secondary students aged 12 to 17 years had never smoked (never even had a puff of a cigarette).
|
12 |
13 |
14 |
15 |
16 |
17 |
12-17 |
|
|
Never smoked |
95.0 |
93.0 |
88.0 |
78.0 |
72.0 |
65.0 |
83.0 |
|
More than 100 cigarettes in lifetime |
<1.0 |
<1.0 |
1.0 |
3.0 |
4.0 |
6.0 |
2.0 |
|
Past year |
3.0 |
5.0 |
9.0 |
17.0 |
23.0 |
28.0 |
13.0 |
|
Past month |
2.0 |
2.0 |
5.0 |
9.0 |
13.0 |
16.0 |
7.0 |
|
Current (past 7 days) |
2.0 |
2.0 |
4.0 |
6.0 |
8.0 |
11.0 |
5.0 |
|
Committed smokers (3+ days in past 7 days) |
1.0 |
1.0 |
2.0 |
3.0 |
4.0 |
6.0 |
3.0 |
Source: Department of Health, Secondary school students’ use of tobacco, alcohol and other drugs in 2017, Table 3.1 Percentage of secondary students in Australia who have smoked in the past week, past month, past year, or lifetime, by age and sex
This survey also reports that five per cent of young people aged 12 to 17 years had smoked in the past week.6
Unsurprisingly the proportion of young people smoking increases as they get older. The lowest proportion of students who had smoked in the past month was 12 and 13 year-olds (2.0%), which increased with age (16.0% for 17 year-olds).
Consistent with the NDSHS survey this survey reported a significant drop in the proportion of Australian high school students smoking from 1999 to 2017. This was across all categories of smoking (ever smoking, smoking in the past year, past month, past week, as well as committed and daily smokers).7
Age of initiation
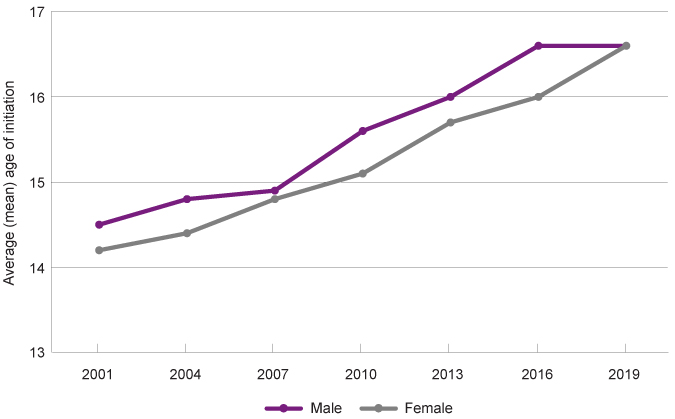
The average age at which Australian young people aged 14 to 24 years smoked their first full cigarette has steadily risen from 14.3 years in 2001 to 16.6 years in 2019.
|
Males |
Females |
Persons |
|
|
2001 |
14.5 |
14.2 |
14.3 |
|
2004 |
14.8 |
14.4 |
14.6 |
|
2007 |
14.9 |
14.8 |
14.9 |
|
2010 |
15.6 |
15.1 |
15.4 |
|
2013 |
16.0 |
15.7 |
15.9 |
|
2016 |
16.6 |
16.0 |
16.3 |
|
2019 |
16.6 |
16.6# |
16.6 |
Source: Australian Institute of Health and Welfare, National Drug Strategy Household Survey 2019, Table 2.11: Age of initiation(a) of tobacco use, people aged 14–24 who have ever smoked a full cigarette, by sex, 2001 to 2019 (years)
# Statistically significant change between 2016 and 2019.
Average (mean) age of initiation of tobacco use for young people aged 14 to 24 years by age in years and gender, age in years, Australia, 2001 to 2019
Source: Australian Institute of Health and Welfare, National Drug Strategy Household Survey 2019, Table 2.11: Age of initiation(a) of tobacco use, people aged 14–24 who have ever smoked a full cigarette, by sex, 2001 to 2019 (years)
In previous years, Australian male young people were generally slightly older than Australian female young people when they smoked their first cigarette. However, in 2019 the average age of initiation across Australia for male and female young people was the same.
From the same survey, the average age of initiation for WA young people aged 14 years to 24 years has also increased from 15.8 in 2007 to 16.5 in 2019, which is similar to the Australian average of 16.6 years in the same year.
|
Age of initiation |
|
|
2007 |
15.8 |
|
2010 |
15.5 |
|
2013 |
15.7 |
|
2016 |
16.6 |
|
2019 |
16.5 |
Source: Australian Institute of Health and Welfare, National Drug Strategy Household Survey 2019, Table S.31: Age of initiation of lifetime drug use, people aged 14 and over, by state/territory, 2007 to 2019 (years)
In SOS19, of the 30.1 per cent of Year 10 to Year 12 WA students who reported they had smoked a cigarette (even just a puff), almost two in five (37.1%) tried their first cigarette when they were under 15 years of age.
|
Years 10 to 12 |
|
|
11 and under |
8.7 |
|
12 to 14 years |
28.4 |
|
15 years and older |
52.6 |
|
I don't remember |
8.9 |
|
Prefer not to say |
1.3 |
Source: Commissioner for Children and Young People WA 2020, Speaking Out Survey 2019 Data Tables [unpublished]
Note: This does not correspond to the ‘age of initiation’ which is generally calculated by including young adults (18 to 24 years) responses regarding when they first started smoking. In the above table, only older students can respond with older age groups, therefore the younger age groups have a higher likelihood of having been selected.
Aboriginal young people
The NDSHS reports that Aboriginal people aged 14 years and over (including adults) are more than twice as likely to smoke tobacco on a daily basis than non-Aboriginal people (24.9% compared to 10.7%). There has however been a steady decrease in the proportion of Aboriginal people smoking on a daily basis over the past decade (34.8% in 2010 compared to 24.9% in 2019).8
In the SOS19 data, Aboriginal students were significantly more likely to have tried cigarette smoking than non-Aboriginal students (32.6% of Aboriginal students had tried compared to 18.9% of non-Aboriginal students).
|
Aboriginal |
Non-Aboriginal |
|
|
No |
58.0 |
77.8 |
|
Yes |
32.6 |
18.9 |
|
Prefer not to say |
9.4 |
3.3 |
Source: Commissioner for Children and Young People WA 2020, Speaking Out Survey 2019 Data Tables [unpublished]
Proportion of Year 7 to Year 12 students who reported whether they have ever tried cigarette smoking, even one or two puffs by Aboriginal status, per cent, WA, 2019
Source: Commissioner for Children and Young People WA 2020, Speaking Out Survey 2019 Data Tables [unpublished]
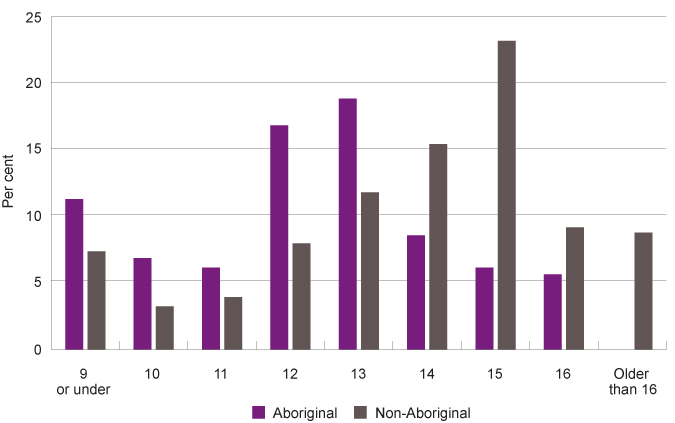
Although the differences were not statistically significant, of the students who had tried smoking, Aboriginal students were more likely than non-Aboriginal students to report smoking at an earlier age.
Proportion of Year 7 to Year 12 students who had ever tried cigarette smoking responding to the question ‘how old were you when you first smoked a cigarette?’ by Aboriginal status, per cent, WA, 2019
Source: Commissioner for Children and Young People WA 2020, Speaking Out Survey 2019 Data Tables [unpublished]
Note: This does not correspond to the ‘age of initiation’ which is generally calculated by including young adults’ (18 to 24 years) responses regarding when they first started smoking. In the above table, only older students can respond with older age groups, therefore the younger ages have a higher likelihood of having been selected.
In 2018–19, the Australian Bureau of Statistics (ABS) conducted the National Aboriginal and Torres Strait Islander Health Survey which included a nationally representative sample of around 10,500 Aboriginal people in remote and non-remote locations.9
In this survey, 9.7 per cent of Aboriginal young people aged 15 to 17 years reported smoking tobacco daily, which was a substantial reduction from the result in 2012–13 of 17.6 per cent.
|
2012-13 |
2018-19 |
|
|
Never smoked |
76.7 |
84.6 |
|
Ex-smoker |
4.3* |
3.6 |
|
Daily smoker |
17.6 |
9.7 |
Source: Australian Bureau of Statistics, National Aboriginal and Torres Strait Islander Health Survey, Australia, 2018–19, Table 11.3 Smoker status by age, sex and Indigenous status, persons aged 15 years and over, 2017–18 and 2018–19, Proportion of persons
* Proportion has a relative standard error between 25 per cent and 50 per cent and should be used with caution
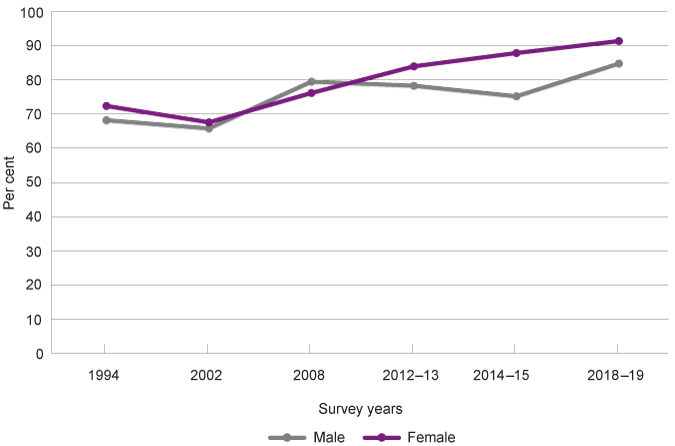
There has been a significant increase in Aboriginal young people not smoking over the last 25 years. In 1994, 70.3 per cent of Aboriginal young people aged 15–17 years did not smoke; by 2018–19 this had increased to 88.2 per cent.
|
1994 |
2002 |
2008 |
2012-13 |
2014-15 |
2018-19 |
|
|
Male |
68.2 |
65.8 |
79.5 |
78.3 |
75.2 |
84.8 |
|
Female |
72.4 |
67.6 |
76.2 |
84.0 |
87.9 |
91.4 |
|
Total |
70.3 |
66.7 |
77.9 |
81.0 |
82.6 |
88.2 |
Source: Australian Bureau of Statistics, 4737.0 - Aboriginal and Torres Strait Islander Peoples: Smoking Trends, Australia, 1994 to 2014-15 and National Aboriginal and Torres Strait Islander Health Survey, Australia, 2018–19
Proportion of Aboriginal young people aged 15 to 17 years not smoking by gender, per cent, Australia, 1994 to 2018–19
Source: Australian Bureau of Statistics, 4737.0 - Aboriginal and Torres Strait Islander Peoples: Smoking Trends, Australia, 1994 to 2014-15 and National Aboriginal and Torres Strait Islander Health Survey, Australia, 2018–19
In general, male Aboriginal young people are more likely to smoke than female Aboriginal young people, although in 2018–19 the proportion of male Aboriginal young people not smoking increased.
Aboriginal young people in remote locations are much more likely to smoke than those in non-remote locations (24.4% in remote locations compared to 10.6% in non-remote locations in 2018–19).10
E-cigarettes
Use of e-cigarettes (vaping) is increasing amongst Australian young people.11 E-cigarettes are devices which aerosolise nicotine or other chemicals which are then inhaled by the user. The liquid solution can be nicotine or THC (a cannabis-based product) or other flavoured solutions.12 THC is illegal in Australia and nicotine is illegal for e-cigarettes.13
In 2019, nearly two-thirds (63.9%) of current smokers aged 18 to 24 years and one-in-five (19.7%) non‑smokers aged 18 to 24 years reported having tried e-cigarettes.14
More data and research is required on the use of e-cigarettes.
Education about tobacco smoking
In SOS19, young people in Years 7 to 12 were asked how much they have learnt about smoking at school. Most (70.6%) young people reported that they had learnt a lot (34.2%) or some (36.4%) about smoking tobacco at school. While, 20.0 per cent reported they had only learnt a little bit and 9.3 per cent reported they had learnt nothing.15
Most (90.6%) high school students reported that they feel like they know enough about the health impacts of smoking, while 5.3 per cent did not feel like they knew enough and 4.1 per cent were not sure.16
Students in remote locations are more likely than those in metropolitan Perth to report that they had learnt a lot about smoking at school (46.1% compared to 32.3%). In spite of this, students in remote locations are less likely to feel like they know enough about the health impacts of smoking than students in the metropolitan region (84.8% compared to 91.6%).17
Lesbian, gay, bisexual, trans and intersex children
For information on LGBTI young people’s consumption of alcohol, tobacco and other drugs refer to the Measure: Use of illicit drugs.
Culturally and linguistically diverse young people
For information on culturally and linguistically diverse young people’s consumption of alcohol, tobacco and other drugs refer to the Measure: Use of illicit drugs.
Young people in the youth justice system
For information on the consumption of alcohol, tobacco and other drugs of young people in youth detention refer to the Measure: Use of illicit drugs.
Endnotes
- Office of the Surgeon General (US) 2004, The Health Consequences of Smoking: A Report of the Surgeon General, Center for Disease Control and Prevention (US), p. 1.
- Khuder et al 1999, Age at smoking onset and its effect on smoking cessation, Addictive behaviours, Vol 24, no 5, p. 95.
- Commissioner for Children and Young People WA 2020, Speaking Out Survey: The views of WA children and young people on their wellbeing - a summary report, Commissioner for Children and Young People WA.
- Commissioner for Children and Young People WA 2020, Speaking Out Survey 2019 Data Tables Commissioner for Children and Young People WA [unpublished].
- Australian Institute of Health and Welfare (AIHW) 2020, National Drug Strategy Household Survey 2019, Table S.9: Daily tobacco smoking status, by age and state/territory, 2007 to 2019, AIHW.
- Guerin N and White V 2018, ASSAD 2017 Statistics & Trends: Australian Secondary Students’ Use of Tobacco, Alcohol, Over-the-counter Drugs, and Illicit Substances, Cancer Council Victoria, p. 15.
- Ibid, p. 16.
- Australian Institute of Health and Welfare 2020, National Drug Strategy Household Survey 2019, Table 8.1: Use of drugs by Indigenous status, people aged 14 and over, 2010 to 2019 (col per cent), AIHW.
- Australian Bureau of Statistics (ABS) 2020, National Aboriginal and Torres Strait Islander Health Survey, 2018-19, Summary results for states and territories (fact sheets), ABS.
- Australian Bureau of Statistics 2020, National Aboriginal and Torres Strait Islander Health Survey, Australia, 2018–19, Table 12.3 Smoker status by age, sex and remoteness, Aboriginal and Torres Strait Islander persons aged 15 years and over, 2004–05 to 2018–19, ABS.
- Australian Institute of Health and Welfare 2020, National Drug Strategy Household Survey 2019, Drug Statistics series no 32, PHE 270, AIHW, p. 10.
- Ibid, p. 9.
- Healthy WA 2021, Electronic cigarettes (e-cigarettes), WA Government [website].
- Australian Institute of Health and Welfare 2020, National Drug Strategy Household Survey 2019, Table 2.19: Lifetime use of electronic cigarettes (e-cigarettes), by age and smoker status and Table 2.20: Lifetime use of electronic cigarettes (e-cigarettes), current smokers, AIHW.
- Commissioner for Children and Young People WA 2020, Speaking Out Survey 2019 Data Tables, Commissioner for Children and Young People WA [unpublished].
- Ibid.
- Ibid.
Last updated August 2021
Illicit drug use is a major cause of preventable disease and illness in Australia. In 2010, WA residents were hospitalised 5,644 times for conditions related to drug use, costing approximately $30m.1
Of all jurisdictions in Australia, WA had the highest rate of unintentional drug-induced deaths in 2018. Furthermore, the rate of unintentional drug-induced deaths in WA increased from 6.4 per 100,000 in 2012 to 8.8 per 100,000 in 2018.2
Aside from the considerable health and behavioural problems associated with illicit drug use, children and young people are at particular risk of harm from drug use, as it negatively impacts the development of neurological pathways and is strongly associated with long-term drug dependency issues.3
In 2019, the Commissioner conducted the Speaking Out Survey (SOS19) which sought the views of a broadly representative sample of 4,912 Year 4 to Year 12 students in WA on factors influencing their wellbeing. In this survey some specific questions were asked of Year 9 to Year 12 students about experiences with illicit drugs.
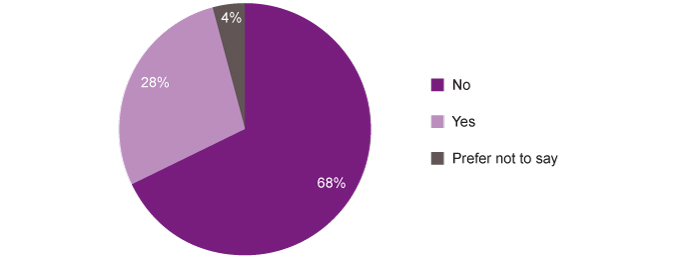
Overall, over one-quarter (28.4%) of young people in Year 9 to Year 12 have had experiences with marijuana. This may include own use as well as use by others, such as friends or family members.
|
Male |
Female |
Metropolitan |
Regional |
Remote |
Total |
|
|
No |
69.2 |
67.1 |
70.0 |
58.8 |
66.0 |
68.2 |
|
Yes |
27.3 |
29.5 |
26.7 |
37.2 |
28.3 |
28.4 |
|
Prefer not to say |
3.5 |
3.5 |
3.2 |
4.0 |
5.7 |
3.5 |
Source: Commissioner for Children and Young People WA 2020, Speaking Out Survey 2019 Data Tables [unpublished]
Proportion of Year 9 to Year 12 students reporting whether they have ever had any experiences with marijuana by various characteristics, per cent, WA, 2019
Source: Commissioner for Children and Young People WA 2020, Speaking Out Survey 2019 Data Tables [unpublished]
Due to the small sample size, differences are not statistically significant, however a greater proportion of young people in regional locations reported that they had experiences with marijuana than in remote and metropolitan areas (37.2% compared to 28.3% and 26.7%).
Of further concern is that one-quarter (26.1%) of Year 10 to Year 12 students thought it was okay for someone their age to use marijuana (compared to 8.2% of Year 7 to Year 9 students). In contrast, fewer (12.7%) Year 10 to Year 12 students thought it was ok for someone their age to smoke tobacco. Additionally, 60.0 per cent of Year 10 to Year 12 students reported that they had friends who used marijuana.4
Overall, more than one in ten (13.4%) young people in Year 9 to Year 12 had had experiences with other drugs (excluding tobacco, alcohol or marijuana).
|
Male |
Female |
Metropolitan |
Regional |
Remote |
Total |
|
|
No |
83.5 |
84.8 |
85.7 |
75.7 |
81.4 |
84.1 |
|
Yes |
14.5 |
12.1 |
12.2 |
20.3 |
12.0 |
13.4 |
|
Prefer not to say |
2.0 |
3.1 |
2.1 |
4.0 |
6.6 |
2.5 |
Source: Commissioner for Children and Young People WA 2020, Speaking Out Survey 2019 Data Tables [unpublished]
Similar to experiences with marijuana, Year 9 to Year 12 students in regional locations were more likely to report that they had had experiences with other drugs than students in metropolitan or remote locations (20.3% compared to 12.2% and 12.0%). There were no differences between male and female students.
Two in five (39.7%) Year 10 to Year 12 students reported that they had friends who used other drugs.5
At the same time, 84.2 per cent of Year 7 to Year 9 students and 59.5 per cent of Year 10 to Year 12 students think young people their age should not use alcohol or other drugs, including tobacco and marijuana.6
The National Drug Strategy Household Survey (NDSHS) is a triennial survey that in 2019 collected information from approximately 23,000 people across Australia. In this survey participants were asked about their drug use patterns, attitudes and behaviours.7
The NDSHS shows a reduction in Australian young people aged 14 to 17 years using illicit drugs from 2010 to 2019 (14.5% of young people in 2010 to 9.7% of young people in 2019).8
The Australian Institute of Health and Welfare (AIHW) reports NDSHS data by jurisdiction, however it has a very high relative standard error and has not been reproduced here. The high sampling error across almost all jurisdictions in recent years is of concern, this suggests that the sample sizes were not sufficient to provide valid and reliable estimates for this critical age group by jurisdiction.
The Australian Secondary Students’ Alcohol and Drug (ASSAD) survey is a triennial national survey of secondary students’ use and attitude towards licit and illicit substances. The 2017 survey included 3,361 WA young people aged from 12 to 17 years from 46 randomly selected government, Catholic and independent schools across the state.9
The following has been produced by the Mental Health Commission reporting WA results from the 2017 ASSAD survey.
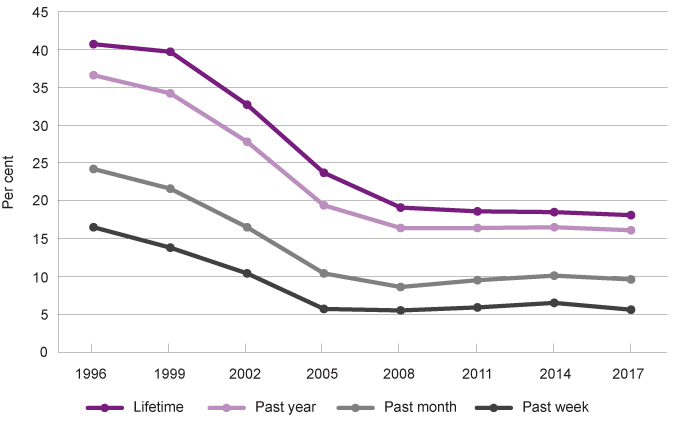
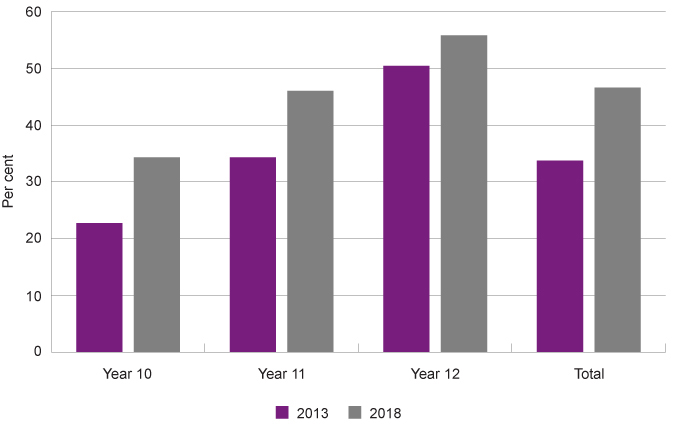
In 2017, less than one in five (18.1%) WA students aged 12 to 17 years reported ever using one illicit drug (including marijuana/cannabis), in comparison to more than two in five (40.7%) students in 1996.10
|
Lifetime |
Past year |
Past month |
Past week |
|
|
1996 |
40.7 |
36.6 |
24.2 |
16.5 |
|
1999 |
39.7 |
34.2 |
21.6 |
13.8 |
|
2002 |
32.7 |
27.8 |
16.5 |
10.4 |
|
2005 |
23.7 |
19.4 |
10.4 |
5.7 |
|
2008 |
19.1 |
16.4 |
8.6 |
5.5 |
|
2011 |
18.6 |
16.4 |
9.5 |
5.9 |
|
2014 |
18.5 |
16.5 |
10.1 |
6.5 |
|
2017 |
18.1 |
16.1 |
9.6 |
5.6 |
Source: Mental Health Commission, Illicit drug trends in Western Australia: Australian school students alcohol and drug survey, Figure 1: Trends in the use of at least one illicit drug, 1996 - 2017
Prevalence and recency of illicit drug use for students aged 12 to 17 years, per cent, WA, 1996 to 2017
Source: Mental Health Commission, Illicit drug trends in Western Australia: Australian school students alcohol and drug survey, Figure 1: Trends in the use of at least one illicit drug, 1996 - 2017
The majority of this decline is due to a reduction in cannabis (marijuana) consumption. Cannabis was the primary illicit drug used by WA young people in 1996, with 39.7 per cent of WA young people in 1996 using cannabis in their lifetime.11 This has reduced to 16.8 per cent of WA young people in 2017.12
There has been a significant decrease in the proportion of young people who had used illicit drugs from 1996 to 2017 in the past year (36.6% to 16.1%), past month (24.2% to 9.6%) and past week (16.5% to 5.6%).13
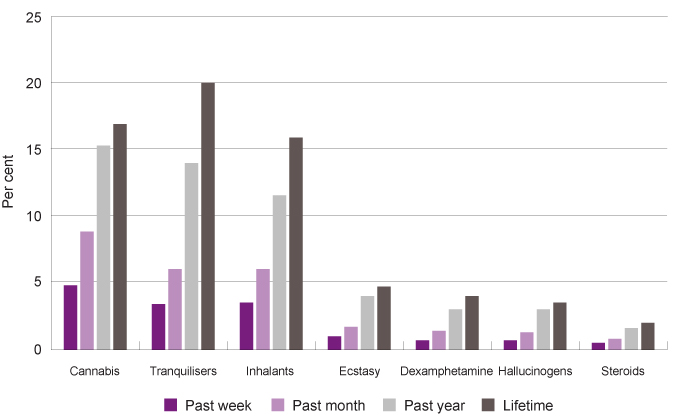
The most commonly used drugs in 2017 among WA young people aged 12 to 17 years in the past year were cannabis (15.2% of all WA 12 to 17 year-olds), tranquilisers (13.9%) and inhalants (11.5%). Tranquilisers include sleeping tablets, sedatives and benzodiazepines, such as Valium, Temazepam and Serepax. While inhalants include substances that are sniffed such as glue, paint or spray cans.
|
Past week |
Past month |
Past year |
Lifetime |
|
|
Cannabis |
4.8 |
8.8 |
15.2 |
16.8 |
|
Tranquilisers* |
3.4 |
6.0 |
13.9 |
19.9 |
|
Inhalants |
3.5 |
6.0 |
11.5 |
15.8 |
|
Ecstasy |
1.0 |
1.7 |
4.0 |
4.7 |
|
Dexamphetamine* |
0.7 |
1.4 |
3.0 |
4.0 |
|
Hallucinogens |
0.7 |
1.3 |
3.0 |
3.5 |
|
Steroids* |
0.5 |
0.8 |
1.6 |
2.0 |
|
Cocaine |
0.4 |
0.7 |
1.2 |
1.6 |
|
Meth/Amphetamines |
0.3 |
0.6 |
0.8 |
1.2 |
Source: Mental Health Commission, Illicit drug trends in Western Australia: Australian school students alcohol and drug survey, Figure 2: Prevalence and recency of illicit drug use for students
* Non-medical use
Prevalence and recency of use of most common illicit drugs for secondary students aged 12 to 17 years, per cent of students, WA, 2017
Source: Mental Health Commission, Illicit drug trends in Western Australia: Australian school students alcohol and drug survey, Figure 2: Prevalence and recency of illicit drug use for students
In the 2017 survey, 65 per cent of young people who used tranquilisers for non-medicinal purposes reported sourcing them from their parents, however, this may include incorrectly reported prescribed use.14
There is limited data comparing WA young people’s drug use to other states or Australia. The data in the below table has been collated from the ASSAD survey in 2017, showing similar results for WA and Australia.
|
Past month |
Lifetime |
|||
|
WA |
Australia |
WA |
Australia |
|
|
Cannabis |
8.8 |
8.0 |
16.8 |
17.0 |
|
Tranquilisers* |
6.0 |
6.0 |
19.9 |
20.0 |
|
Inhalants |
6.0 |
8.0 |
15.8 |
18.0 |
|
Ecstasy |
1.7 |
2.0 |
4.7 |
6.0 |
|
Dexamphetamine* |
1.4 |
1.0 |
4.0 |
2.0 |
|
Hallucinogens |
1.3 |
1.0 |
3.5 |
4.0 |
|
Steroids* |
0.8 |
1.0 |
2.0 |
3.0 |
|
Cocaine |
0.7 |
1.0 |
1.6 |
2.0 |
|
Meth/amphetamines |
0.6 |
1.0 |
1.2 |
2.0 |
Source: Mental Health Commission, Illicit drug trends in Western Australia: Australian school students’ alcohol and drug survey, and National Drug Strategy, Australian secondary school students’ use of tobacco, alcohol, and over-the-counter and illicit substances in 2017
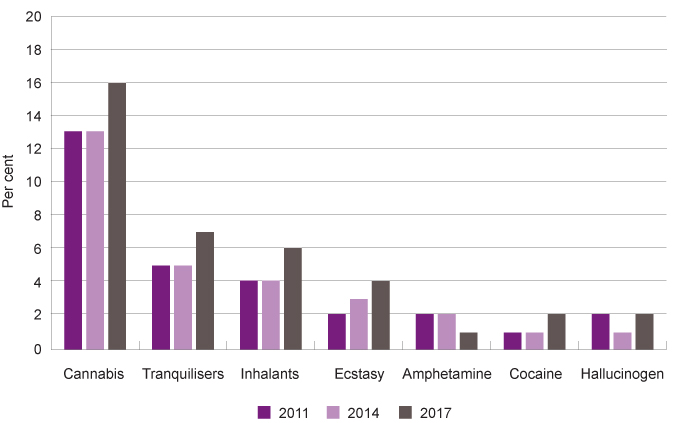
For each of the most common illicit drugs, except inhalants, Australian young people aged 16 to 17 years are more likely to have used drugs in the past month than young people aged 12 to 15 years.
|
12 to 15 years |
16 to 17 years |
|||||
|
2011 |
2014 |
2017 |
2011 |
2014 |
2017 |
|
|
Cannabis |
4.0 |
5.0 |
5.0 |
13.0# |
13.0 |
16.0 |
|
Tranquilisers |
4.0# |
5.0 |
5.0 |
5.0# |
5.0 |
7.0 |
|
Inhalants |
8.0 |
7.0 |
8.0 |
4.0# |
4.0# |
6.0 |
|
Ecstasy |
1.0 |
1.0 |
1.0 |
2.0# |
3.0 |
4.0 |
|
Amphetamine |
1.0 |
1.0 |
1.0 |
2.0 |
2.0 |
1.0 |
|
Cocaine |
<1.0 |
1.0 |
1.0 |
1.0 |
1.0 |
2.0 |
|
Opiate |
1.0 |
1.0 |
1.0 |
1.0 |
1.0 |
1.0 |
|
Hallucinogen |
1.0 |
1.0 |
1.0 |
2.0 |
1.0 |
2.0 |
|
Steroids |
1.0 |
1.0 |
1.0 |
1.0 |
1.0 |
1.0 |
Source: National Drug Strategy, Australian secondary school students’ use of tobacco, alcohol, and over-the-counter and illicit substances in 2017
# Significantly different from the 2017 result
Young people aged 16 to 17 years, use of most common illicit drugs in the past month, per cent, Australia, 2011, 2014 and 2017
Source: National Drug Strategy, Australian secondary school students’ use of tobacco, alcohol, and over-the-counter and illicit substances in 2017
The above age breakdown is not published for WA young people, although it is likely the trends will be similar.
Data for Australian young people aged 16 to 17 years highlights a recent increase in usage of the most common drugs, except amphetamine, from 2014 to 2017.15 These results will continue to be monitored to determine if they represent an ongoing trend.
Interestingly, amphetamine use has been decreasing for high school students in WA since 2002.16 These statistics contrast with concerns surrounding a current ‘ice epidemic’ in Australia. Data shows that while across Australia there has not been an increase in users of amphetamines (including ‘speed’ and ‘ice’), there has been an increase in hospitalisations related to methamphetamine use.17 Research suggests that existing amphetamine users are switching from ‘speed’ to ‘ice’, which is a purer form of amphetamine that causes more harm.18 It is believed that this is because price reductions have increased the availability of methamphetamine with higher purity, which is more harmful.19,20
The 2017 ASSAD survey shows that Australian male young people aged 12 to 17 years are slightly more likely to use illicit drugs (including non-prescribed tranquilisers) than female young people, although in the case of most drugs there was minimal difference.21
The NDSHS collects information on the factors that influence young people to use an illicit drug.
|
2013 |
2016 |
2019 |
|
|
To see what it was like/curiosity |
70.7 |
64.3 |
65.7 |
|
Friends or family member were using it/ offered by friend or family member |
39.4 |
45.0 |
49.0 |
|
To do something exciting |
30.3 |
22.1 |
24.6 |
|
Thought it would improve mood/to stop feeling unhappy |
20.9 |
17.8* |
23.4 |
|
To enhance an experience |
11.5* |
17.9* |
16.2* |
|
Other |
3.2** |
4.7** |
3.4** |
Source: Australian Institute of Health and Welfare, National Drug Strategy Household Survey 2019, Table 4.22: Factors influencing first use of an illicit drug, people who have used an illicit drug in their lifetime(a), by age and use status, 2013 to 2019 (per cent)
* Estimate has a relative standard error of 25 per cent to 50 per cent and should be used with caution.
** Estimate has a high level of sampling error (relative standard error of 51% to 90%), meaning that it is unsuitable for most uses.
Note: Respondents could select more than one response.
The most commonly cited reason for Australian young people aged 14 to 17 years to use illicit drugs for the first time was to see what it was like and/or curiosity (65.7%). A significant proportion (49.0%) of young people were also influenced by friends or family who were using it or they were offered it by a friend or family member.
Critically, almost one-quarter (23.4%) of Australian young people aged 14 to 17 years took illicit drugs for the first time because they thought it would improve their mood or stop them feeling unhappy.
There was no further disaggregation by gender, Aboriginal status or geographic location for this data.
Aboriginal young people
In SOS19, a significantly lower proportion of Aboriginal students than non-Aboriginal students reported not having had experiences with marijuana (55.6% compared to 68.8%).
It should be noted that experiences with a drug will often include being around people who are using the drug at a party, gathering or at home.
|
Experiences with marijuana |
Experiences with other drugs |
|||
|
Aboriginal |
Non-Aboriginal |
Aboriginal |
Non-Aboriginal |
|
|
No |
55.6 |
68.8 |
78.8 |
84.3 |
|
Yes |
34.9 |
28.0 |
15.0 |
13.3 |
|
Prefer not to say |
9.5 |
3.2 |
6.2 |
2.4 |
Source: Commissioner for Children and Young People WA 2020, Speaking Out Survey 2019 Data Tables [unpublished]
Similar proportions of Aboriginal and non-Aboriginal young people reported having had experiences with other drugs.
The results are not statistically significant, but marginally higher proportions of Aboriginal than non-Aboriginal young people reported thinking it is okay for someone their age to use cigarettes/tobacco or other drugs.
|
Aboriginal |
Non-Aboriginal |
|
|
Cigarettes, tobacco |
11.8 |
7.9 |
|
Alcohol |
18.4 |
17.9 |
|
Marijuana |
17.3 |
16.6 |
|
Other drugs |
10.4 |
7.1 |
|
None |
72.1 |
72.7 |
Source: Commissioner for Children and Young People WA 2020, Speaking Out Survey 2019 Data Tables [unpublished]
Note: the students were able to choose as many as they needed.
There is limited data on Aboriginal young people’s use of illicit or other drugs. However, the data suggests that illicit drug use is similar among Aboriginal and non-Aboriginal young people.
In 2020, the Australian Bureau of Statistics (ABS) released results for the National Aboriginal and Torres Strait Islander Health (NATSIH) Survey. Based on this survey, in 2018–19, 32.9 per cent of Aboriginal people aged 15 to 29 years had used a drug for non-medical purposes in the last 12 months.22 This survey does not report separately on Aboriginal children and young people.
The NDSHS reports that in 2019, a similar proportion (31.2%) of 18 to 24 year old Australian young people have recently used illicit drugs.23
In the NATSIH Survey, drug use is sustained at 31.0 per cent for Aboriginal people aged 30 to 44 years. While, in the NDSHS, drug use for 30 to 39 year-old Australians decreases to 19.1 per cent. 24,25
Therefore, while illicit drug use is estimated to be similar among Aboriginal and non-Aboriginal young people, the data shows that Aboriginal people continue using into adulthood at higher levels than non-Aboriginal people. This is related to the burden of inter-generational trauma, disconnection from communities, cultural values and traditions as a result of the ongoing effects of colonisation.26
Aboriginal people are also more likely than non-Aboriginal people to experience significant life stressors. For example, in the ABS Australian Aboriginal and Torres Strait Islander Health Survey, Aboriginal young people aged 15 to 24 years are more likely than non-Aboriginal young people to have experienced a death of a family member (30.9% compared to 21.1%) and been unable to get a job (24.3% compared to 11.7%).27
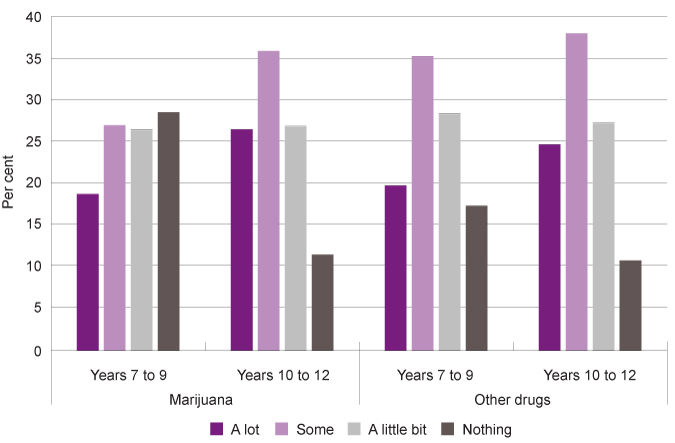
Education about marijuana and other illicit drugs
In SOS19 students in Year 7 to Year 12 were asked how much they have learnt about marijuana and other drugs at school.
Almost one-half (46.9%) of Year 7 to Year 12 students reported that they had learnt a little bit (26.5%) or nothing (20.4%) about marijuana at school. This is in contrast to the proportion of students who reported learning a little bit or nothing about alcohol (23.0%) and smoking (29.4%).
Students in Years 10 to 12 had learnt more than students in Year 7 to 9 about marijuana at school, but a significant proportion (38.1%) of older students still reported they had learnt a little bit (27.1%) or nothing (10.7%).
Similarly, a large proportion (41.8%) of students in Year 7 to Year 12 had learnt a little bit (27.7%) or nothing (14.1%) about other drugs at school.
|
Marijuana |
Other drugs |
|||||
|
Years 7 to 9 |
Years 10 to 12 |
All |
Years 7 to 9 |
Years 10 to 12 |
All |
|
|
A lot |
18.6 |
26.3 |
22.2 |
19.6 |
24.5 |
21.9 |
|
Some |
26.8 |
35.6 |
30.9 |
35.0 |
37.7 |
36.3 |
|
A little bit |
26.3 |
26.7 |
26.5 |
28.2 |
27.1 |
27.7 |
|
Nothing |
28.3 |
11.4 |
20.4 |
17.2 |
10.7 |
14.1 |
Source: Commissioner for Children and Young People WA 2020, Speaking Out Survey 2019 Data Tables [unpublished]
Proportion of Year 7 to Year 12 students reporting how much they have learnt about marijuana and other drugs at school by year group, per cent, WA, 2019
Source: Commissioner for Children and Young People WA 2020, Speaking Out Survey 2019 Data Tables [unpublished]
Thus, although more students are learning about marijuana and other drugs as they move through school, a significant proportion are not learning very much even by the time they reach Years 10 to 12.
Notably, one in five (21.9%) Year 7 to Year 12 students reported that they did not feel like they knew enough about the health impacts of marijuana and 12.5 per cent were not sure. That is, one-third (34.4%) of WA high school students do not feel like they know enough (or are not sure) about the health impacts of marijuana.
|
Male |
Female |
Metropolitan |
Regional |
Remote |
Total |
|
|
No |
18.9 |
25.4 |
23.4 |
15.1 |
16.6 |
21.9 |
|
Yes |
71.9 |
59.1 |
64.6 |
72.0 |
64.6 |
65.6 |
|
I'm not sure |
9.3 |
15.6 |
12.0 |
12.9 |
18.8 |
12.5 |
Source: Commissioner for Children and Young People WA 2020, Speaking Out Survey 2019 Data Tables [unpublished]
A greater proportion of female students than male students did not feel like they knew enough or were not sure about the health impacts of marijuana (41.0% compared to 28.2%).
Similarly, 29.1 per cent of students in Year 7 to Year 12 reported that they do not feel like they know enough or are not sure about the health impacts of other drugs.28
Aboriginal and non-Aboriginal students reported similar experiences of learning about drugs at school and feeling like they know enough about the health impacts.29
Lesbian, gay, bisexual, trans and intersex young people
Lesbian, gay, bisexual, transgender and intersex (LGBTI)30 children and young people are at an increased risk of the consumption of tobacco, alcohol or illicit drugs
Having a diverse sexual orientation, diverse gender identity, or being intersex are not in themselves risk factors for tobacco use, alcohol consumption or illicit drug use. However, the issues that affect LGBTI people such as social and cultural beliefs and assumptions about gender and sexuality, including systemic discrimination at an individual, social, political and legal level mean that young people within this group may use alcohol, tobacco and illicit drugs as a form of self-medication.31
The 2019 NDSHS reported relatively high rates of alcohol, tobacco and illicit drug use among same sex attracted or bisexual participants aged 14 years and older (including adults). Same-sex attracted/bisexual respondents were more likely to consume alcohol on a single occasion at least monthly at levels that were risky (35.4% of same-sex attracted/bisexual participants compared to 26.1% of heterosexual participants) and more likely to smoke tobacco on a daily basis (16.7% compared to 10.8%).32
Furthermore, almost two in five (36.0%) same-sex attracted/bisexual respondents reported that they had recently used an illicit drug, compared to 16.1 per cent of heterosexual respondents. The most common illicit drugs recently used by same-sex attracted/bisexual respondents were cannabis (25.9%), inhalants (9.9%), cocaine (8.0%) and ecstasy (7.4%).33 The NDSHS does not provide data for same-sex attracted/bisexual young people or LGBTI young people, more broadly.
In 2019, La Trobe University conducted the Writing themselves In 4 national survey with 6,418 LGBTI young people aged 14 to 21 years.34 The study does not report on a representative sample of the LGBTI community in Australia, however does provide valuable insights into the experiences of young people within the LGBTI community.
This survey found that less than one-half (47.7%) of participants aged 14 to 17 years reported drinking alcohol, which the authors note is a lower proportion than in the general population. Further, the study reported that 85.2 per cent of LGBTI young people aged 14 to 17 years had never smoked, while 11.5 per cent currently smoke. Again, this is lower than the general population for that age group.35
This survey found that LGBTI young people reported much lower levels of alcohol and tobacco smoking than in the previous 2010 Writing themselves In 3 survey.36
In contrast, the participants did report higher levels of illicit drug use than the non-LGBTI young people, with over one-quarter (26.5%) of LGBTI young people aged 14 to 17 years reported using drugs for non-medicinal purposes in the past six months,37 compared to the NDSHS which found that 9.7 per cent of young people aged 14 to 17 years had used an illicit drug in the previous 12 months.38
The most commonly used drug (for non-medicinal purposes) by LGBTI young people aged 14 to 17 years was cannabis (22.2%) followed by anti-depressants (5.0%).39
Male young people (both trans and cisgender) were more likely to use illicit drugs than female trans and cisgender young people.40
For more information on LGBTI children and young people, refer to the Commissioner’s 2018 issues paper: Lesbian, Gay, Bisexual, Trans and Intersex (LGBTI) children and young people.
Culturally and linguistically diverse young people
Some children and young people from CALD backgrounds (and their families) experience language barriers, feeling torn between cultures, intergenerational conflict, racism and discrimination, bullying and resettlement stress.41 Refugee young people are at a higher risk of substance misuse due to dealing with loss, trauma, settlement issues, low socioeconomic status, family breakdowns, intergenerational conflict, youth unemployment, difficulties in school, peer influence, desire for acceptance and the lack of culturally appropriate social and recreational activities.42,23
Data and research also suggests that people from culturally and linguistically diverse (CALD) backgrounds often do not seek help for mental health issues.44 For some, the use of legal and illicit drugs can be a way of coping with these challenges.45 However, there are many protective factors that assist in reducing substance misuse within the CALD and refugee community. These protective factors include spiritual beliefs, cultural norms, and strong community connections.46
There is limited data on substance misuse of CALD young people, however the data that is available suggests that across all age groups they are less likely to consume alcohol, tobacco and illicit drugs than other Australian people.
The 2019 NDSHS compared the proportion of drug use between English and language other than English (LOTE) speakers aged 14 years and older (including adults).47 The data highlights that a low proportion of LOTE participants (6.2%) are daily smokers in comparison to English speaking participants (11.8%).48 Similarly, 52.9 per cent of LOTE Australians did not drink alcohol, compared to 19.2 per cent of non-LOTE Australians. While, 82.6 per cent of LOTE Australians had never used an illicit drug compared to 51.6 per cent of non-LOTE Australians.49
For more information on CALD children and young people and their wellbeing concerns, refer to the Commissioner’s 2016 ‘This is Me’ paper: Stories from culturally and linguistically diverse children and young people.
Young people in the youth justice system
Children and young people in the youth justice system are more likely to have mental health issues which increases the risk of substance use.50 The Banksia Hill Detention Centre is the only facility in WA for the detention of children and young people 10 to 17 years of age who have been remanded or sentenced to custody.
During 2019–20, approximately 107 children and young people aged between 10 and 17 years were held in the Banksia Hill Detention Centre in WA on an average day.51
In their 2021 inspection of the Banksia Hill facility, the Office of the Inspector of Custodial Services noted that although the young people entering the centre were often drug-affected, alcohol and other drug counselling services were not available because federal funding had been cut.52
Children and young people entering youth detention have the right to be assessed to determine whether they have a physical or intellectual disability, mental health issues, alcohol and other drug issues or experience other forms of vulnerability and to have those needs met.
No data is available on alcohol, tobacco or illicit drugs consumption of WA young people in the youth justice system.
In 2015 the Young People in Custody Health Survey (YPICHS) was conducted in NSW across seven juvenile justice centres. Of the young people invited to participate, 90.4 per cent completed the survey which represented 59.3 per cent of young people in custody at the time across NSW.53
Results from this survey highlighted an overwhelming majority of young people in custody smoked tobacco. Over nine in ten (92.0%) survey participants reported that they had smoked in their lifetime, and four in five participants (85.4%) stated that they had smoked in the last 12 months.54 There were no significant differences in gender or Aboriginality among those who had reported smoking more than 20 cigarettes per day, however, the mean age of smoking initiation among Aboriginal young people was significantly earlier than non-Aboriginal young people (11.7 years and 12.7 years respectively).55
These results are in contrast to the broader population of Australian young people aged 12 to 17 years where 83.0 per cent have never smoked,56 and the average age of initiation was around 16 years of age.57
Alcohol consumption in the lifetime of the young people in custody was reportedly over nine in ten participants (93.4%), and of those young people, 96.7 per cent had experienced being drunk, with no gender or Aboriginality differences.58 Age of initiation of a young person’s first full serve of alcohol did not differ between male and female young people (13.1 years and 13.4 years), however Aboriginal young people reported initiation at a significantly earlier age (12.7 years).59 Two in five young people who participated in the survey reported getting drunk weekly prior to custody and just over half of the young people had stated that drinking alcohol had contributed to problems with school, health, friends and family.60
Of those who participated in the survey, a very high 92.5 per cent of young people reported using an illicit drug in their lifetime, there were no gender or Aboriginality differences.61 The most common illicit drugs were cannabis (90.2%), methamphetamine (55.1%) and ecstasy (41.8%).62 Notably, results highlighted the prevalence of methamphetamine had tripled since 2009, which was 17.7 per cent and had increased to 55.1 per cent in 2015.63
Between 2012 and 2016 the AIHW compiled a report which contains data from the Alcohol and Other Drug Treatment Services National Minimum Data Set (AODTS NMDS) and the Juvenile National Minimum Data Set.64 This longitudinal data collected information on demographics of young people aged 10 to 17 years who were under youth justice supervision and/or had been publicly funded to receive an alcohol or other drug treatment service.65
It was found that those young people in Australia who were currently under youth justice supervision were thirty times more likely to have accessed an alcohol or drug treatment service in comparison to the rest of the young people in the Australian population.66
Endnotes
- Miller J et al 2012, Australian School Student Alcohol and Drug Survey: Illicit Drug Report 2011 – Western Australian results, Surveillance Report Number 9, Drug and Alcohol Office, WA Government, p. 1.
- Penington Institute 2020, Australia’s Annual Overdose Report 2020, Penington Institute.
- Whyte AJ et al 2018, Editorial: Long-Term Consequences of Adolescent Drug Use: Evidence From Pre-clinical and Clinical Models, frontiers in behavioral neuroscience, Vol 12, No 83.
- Commissioner for Children and Young People WA 2020, Speaking Out Survey 2019 Data Tables, Commissioner for Children and Young People WA [unpublished].
- Ibid.
- Ibid.
- Australian Institute of Health and Welfare (AIHW) 2017, National Drug Strategy Household Survey 2016: detailed findings, Drug Statistics series no 31 Cat no PHE 214, AIHW, p. 3 and 134.
- Australian Institute of Health and Welfare 2020, National Drug Strategy Household Survey 2019 data, Table S.28: Recent illicit use of any drug(a), by age and state/territory, 2007 to 2019 (per cent), AIHW.
- WA Mental Health Commission (MHC) 2019, Bulletin: Illicit drug trends in Western Australia: Australian school students alcohol and drug survey - 2017, MHC.
- Ibid.
- Miller J et al 2012, Australian School Student Alcohol and Drug Survey: Illicit Drug Report 2011–Western Australian results, Drug and Alcohol Office Surveillance Report: Number 9. Drug and Alcohol Office, WA Government.
- WA Mental Health Commission (MHC) 2019, Bulletin: Illicit drug trends in Western Australia: Australian school students alcohol and drug survey - 2017, MHC.
- Ibid.
- Guerin N and White V 2018, ASSAD 2017 Statistics & Trends: Australian Secondary Students’ Use of Tobacco, Alcohol, Over-the-counter Drugs, and Illicit Substances, Cancer Council Victoria, p. 28.
- In contrast the AIHW National Drug Strategy Household Survey (NDSHS) shows a decrease across all states in illicit drug use from 2013 to 2016 for young people aged 12 to 17 years. There may be multiple reasons for this, including differing time periods, the NDSHS survey does not include the misuse of prescription drugs such as tranquilisers in the illicit drugs category and the age groups differ.
- Miller J et al 2012, Amphetamine-type Stimulants in Western Australia: ASSAD Survey 2011, Brief communication no 5, Drug and Alcohol Office, WA Government.
- Allan J et al 2019, Increased demand for methamphetamine treatment in rural Australia, Addiction Science and Clinical Practice, Vol 14, No 13.
- Roche A et al 2015, Methamphetamine use in Australia, National Centre for Education and Training on Addiction (NCETA), Flinders University.
- Lim M et al 2014, ‘Ice epidemic’? Trends in methamphetamine use from three Victorian surveillance systems, Australian and New Zealand Journal of Public Health, Vol 39 No 2.
- Scott N et al 2015, High-frequency drug purity and price series as tools for explaining drug trends and harms in Victoria, Australia, Addiction, Vol 110 No 1.
- Guerin N and White V 2018, ASSAD 2017 Statistics & Trends: Australian Secondary Students’ Use of Tobacco, Alcohol, Over-the-counter Drugs, and Illicit Substances. Cancer Council Victoria, 2018.
- Australian Bureau of Statistics (ABS) 2020, National Aboriginal and Torres Strait Islander Health Survey: 2018-19, Table 15.3 Substance use by age, remoteness and sex, Aboriginal and Torres Strait Islander persons aged 15 years and over, 2018–19, ABS.
- Australian Institute of Health and Welfare (AIHW) 2020, National Drug Strategy Household Survey 2019 data, Table 4.8: Recent(a) illicit use of drugs, by age and sex, 2001 to 2019 (per cent), AIHW.
- Australian Bureau of Statistics (ABS) 2020, National Aboriginal and Torres Strait Islander Health Survey: 2018-19, Table 15.3 Substance use by age, remoteness and sex, Aboriginal and Torres Strait Islander persons aged 15 years and over, 2018–19, ABS.
- Australian Institute of Health and Welfare (AIHW) 2020, National Drug Strategy Household Survey 2019 data, Table 4.8: Recent(a) illicit use of drugs, by age and sex, 2001 to 2019 (per cent), AIHW.
- National Indigenous Drug and Alcohol Committee 2014, Alcohol and other drug treatment for Aboriginal and Torres Strait Islander peoples, Australian National Council on Drugs, p. 5.
- Australian Bureau of Statistics, Australian Aboriginal and Torres Strait Islander Health Survey: First Results, Australia, 2012-13, Table 19.3 Selected family stressors(a) by age, Indigenous status and sex, Proportion of persons.
- Commissioner for Children and Young People WA 2020, Speaking Out Survey 2019 Data Tables, Commissioner for Children and Young People WA [unpublished].
- Ibid.
- The Commissioner for Children and Young People understands there are a range of terms and definitions that people use to define their gender or sexuality. The Commissioner’s office will use the broad term LGBTI to inclusively refer to all people who are lesbian, gay, bisexual, trans and intersex, as well as to represent other members of the community that use different terms to describe their diverse sexuality and/or gender.
- Hillier L et al 2010, Writing Themselves in 3: The third national study on the sexual health and wellbeing of same sex attracted and gender questioning young people, Australian Research Centre in Sex, Health and Society, La Trobe University, p. 54.
- Australian Institute of Health and Welfare (AIHW) 2020, National Drug Strategy Household Survey 2019: Data – Chapter 8 Specific Population Groups, Table 8.4: Use of drugs by sexuality, people aged 14 and over, 2010 to 2019 (age standardised per cent), AIHW.
- Ibid.
- Survey conducted with 6,418 Australian LGBTI young people aged 14 to 21 years old were provided access to an online questionnaire with both quantitative and qualitative questions regarding their sexual health and wellbeing.
- Hill A et al 2021, Writing Themselves In 4: The health and wellbeing of LGBTQA+ young people in Australia - National report, La Trobe University, p. 104.
- Ibid, p. 104.
- Ibid, p. 105.
- Australian Institute of Health and Welfare 2020, National Drug Strategy Household Survey 2019 data, Table S.28: Recent illicit use of any drug(a), by age and state/territory, 2007 to 2019 (per cent), AIHW.
- Hill A et al 2021, Writing Themselves In 4: The health and wellbeing of LGBTQA+ young people in Australia - National report, La Trobe University, p. 105.
- Ibid, p. 106.
- WA Office of Multicultural Interests 2009, Not drowning, waving: Culturally and linguistically diverse young people at risk in Western Australia, p. 5.
- Ibid, p. 5.
- Foundation House and Centre for Multicultural Youth 2013, Responding to challenges of misuse of alcohol and other drugs by young people of refugee backgrounds: Reflections from two projects, Foundation House and Centre for Multicultural Youth, p. 4-5.
- Australian Department of HealthHealth 2020, Fact sheet: Mental health services for people of culturally and linguistically diverse (CALD) backgrounds, Australian Government.
- WA Office of Multicultural Interests 2009, Not drowning, waving: Culturally and linguistically diverse young people at risk in Western Australia, WA Government, p. 5.
- Ibid, p. 36.
- Australian Institute of Health and Welfare (AIHW) 2020, National Drug Strategy Household Survey 2019: Data – Chapter 8 Specific Population Groups, Table 8.20: Use of drugs by main language spoken at home, people aged 14 and over, 2010 to 2019 (age standardised col per cent), AIHW.
- Ibid.
- Ibid.
- Justice Health & Forensic Mental Health Network and Juvenile Justice NSW 2015, 2015 Young People in Custody Health Survey: Full Report, NSW Government, p. 65.
- WA Department of Justice 2020, Annual Report: 2019–20, WA Government, p. 34.
- Office of the Inspector of Custodial Services 2021, 2020 Inspection of Banksia Hill Detention Centre, WA Government, p. 22 & 48.
- Justice Health & Forensic Mental Health Network and Juvenile Justice NSW 2015, 2015 Young People in Custody Health Survey: Full Report, NSW Government, p. xx.
- Ibid, p. 56-57.
- Ibid, p. 56-57.
- Department of Health, Secondary school students’ use of tobacco, alcohol and other drugs in 2017, Table 3.1 Percentage of secondary students in Australia who have smoked in the past week, past month, past year, or lifetime, by age and sex.
- Australian Institute of Health and Welfare, Alcohol, tobacco and other drugs in Australia: Populations, Table S3.31 Age of initiation of tobacco use, people aged 14-24, 1995 to 2016 (years).
- Justice Health & Forensic Mental Health Network and Juvenile Justice NSW 2015, 2015 Young People in Custody Health Survey: Full Report, NSW Government, p. 58.
- Ibid, p. 58.
- Ibid, p. 58.
- Ibid, p. 60.
- Ibid, p. 61.
- Ibid, p. 94.
- Australian Institute of Health and Welfare (AIHW) 2018, Overlap between youth justice supervision and alcohol and other drug treatment services 2012–16, Cat no JUV 126, AIHW, p. 1.
- Ibid, p. 1.
- Ibid, p. 14.
Last updated August 2021
Sexual development and experimentation is a normal and healthy part of adolescence. However, there are risks associated with sexual activities and it is critical that young people are well informed and supported to make healthy choices. Adolescence is also a time where young people engaging in intimate relationships can encounter issues related to consent, respect and gender stereotypes.1
To develop effective policies in the area of sexual health it is critical that government and service providers have a realistic understanding of the knowledge and behaviours of young people. It is important for young people to have strong and positive connections with supportive adults who they can ask for help or guidance when they are concerned or worried about their relationships and/or about sex. It is also critical that young people can openly and comfortably communicate boundaries and concerns with sexual partners to reduce unsafe or unwanted sexual activity.2
This section does not consider sexting or negative online experiences in any detail, these topics are discussed in the Safe in the community indicator.
In 2019, the Commissioner conducted the Speaking Out Survey (SOS19) which sought the views of a broadly representative sample of 4,912 Year 4 to Year 12 students in WA on factors influencing their wellbeing, including a range of questions on relationships and intimacy for the older students.3
Overall, one-quarter (24.1%) of young people in Years 9 to 12 reported that they had been with someone in an intimate or sexual way that included having sexual intercourse.
|
Male |
Female |
Metropolitan |
Regional |
Remote |
All |
|
|
No |
69.9 |
68.4 |
70.6 |
61.3 |
66.7 |
69.1 |
|
Yes |
22.7 |
25.6 |
22.6 |
32.8 |
22.2 |
24.1 |
|
Prefer not to say |
7.4 |
6.0 |
6.8 |
5.8 |
11.1 |
6.8 |
Source: Commissioner for Children and Young People WA 2020, Speaking Out Survey 2019 Data Tables [unpublished]
Year 9 to Year 12 students in regional locations were more likely than metropolitan and remote areas to report that they had had sexual intercourse, although this difference was not statistically significant (32.8% compared to 22.6% and 22.2%).
Disaggregation by age shows that 15.3 per cent of Year 9 and 10 students and one-third (34.1%) of Years 11 and 12 students have had sexual intercourse.
|
Years 9 to 10 |
Years 11 to 12 |
|
|
No |
78.0 |
59.1 |
|
Yes |
15.3 |
34.1 |
|
Prefer not to say |
6.8 |
6.8 |
Source: Commissioner for Children and Young People WA 2020, Speaking Out Survey 2019 Data Tables [unpublished]
Proportion of Year 9 to Year 12 students reporting whether they have been with someone in an intimate or sexual way that included having sexual intercourse or going all the way by year group, per cent, WA, 2019
Source: Commissioner for Children and Young People WA 2020, Speaking Out Survey 2019 Data Tables [unpublished]
The Australian Study of Health and Relationships (ASHR) survey is conducted every ten years and provides a snapshot of the sexual health and wellbeing of the Australian population. Key findings of the survey conducted between October 2012 and November 2013 highlighted that the Australian median age of first vaginal intercourse was 17 years.4 The age of initiation differed with sexual identity, with LGBTI male and female young people reporting later ages of first vaginal intercourse, where relevant.5
Historically, the median age of first vaginal intercourse decreased significantly from the 1950s to the 1970s and since the mid-1980s has been mostly stable at 17 years of age for both men and women.6
The National Survey of Australian Secondary Students and Sexual Health is a survey conducted every five years that collects the sexual attitudes, knowledge and experiences of high school students in Years 10 to 12 across Australia. The 2018 survey had a sample of 6,327 Australian students, including 563 WA students. Australia-wide, 3.9 per cent of the sample reported being Aboriginal. Students in metropolitan and inner regional areas were overrepresented.7 While the sample aligned demographically with the census data the researchers note that they ‘cannot say it is representative of all secondary students in Australia’ due to the sampling approach (including sampling bias and self-selection bias).8
Approximately almost one-half (46.6%) of Year 10 to Year 12 students reported ever having vaginal or anal intercourse.9 This is a significant increase on the 2013 survey, which reported that 33.7 per cent of participants had had sexual intercourse.10
|
2013 |
2018 |
|
|
Year 10 |
22.7 |
34.3 |
|
Year 11 |
34.3 |
46.0 |
|
Year 12 |
50.4 |
55.8 |
|
Total |
33.7 |
46.6 |
Source: La Trobe University, National Survey of Australian Secondary Students and Sexual Health 2013, Table 5.4 Students who have ever had sexual intercourse by year level and National Survey of Australian Secondary Students and Sexual Health 2018, Table 5.13 Students who have ever had sexual intercourse (anal and/or vaginal) by year level
Proportion of students who have ever had sexual intercourse (vaginal and/or anal), per cent, Australia, 2013 and 2018
Source: La Trobe University, National Survey of Australian Secondary Students and Sexual Health 2013, Table 5.4 Students who have ever had sexual intercourse by year level and National Survey of Australian Secondary Students and Sexual Health 2018, Table 5.13 Students who have ever had sexual intercourse (anal and/or vaginal) by year level
The disaggregation by year group shows that just over one in three (34.3%) Year 10 students having had sexual intercourse, almost one-half of (46.0%) Year 11 students and over one-half of (55.8%) Year 12 students.
For most of these young people (64.6%), their most recent sexual encounter was with their current steady girlfriend or boyfriend. A smaller, but still significant proportion (28.9%) reported that their last encounter was with someone they had known for a while.11
Students who had not had sexual intercourse reported various reasons for this including: they ‘did not feel ready to have sex’ (67.5% high importance), they were ‘proud to say No and mean it’ (79.1% high importance), and/or that they thought it was ‘important to be in love the first time’ (57.9% high importance).12 Ninety‑five per cent of non-sexually active students reported they did not feel at all guilty, while 81.9 per cent of non-sexually active students reported they did not feel at all embarrassed.13
The majority of young people in the survey had engaged in some form of sexual activity.
|
Male |
Female |
Trans and |
Total |
|
|
Deep kissing |
69.4 |
78.3 |
70.8 |
74.4 |
|
Touching a partner's genitals |
62.7 |
66.9 |
64.1 |
65.0 |
|
Being touched on the genitals |
61.6 |
68.7 |
64.1 |
65.6 |
|
Touching your own genitals |
96.4 |
82.9 |
88.7 |
89.0 |
|
Giving oral sex |
47.1 |
56.2 |
46.2 |
52.1 |
|
Receiving oral sex |
49.4 |
53.0 |
43.1 |
51.4 |
|
Anal sex |
14.3 |
11.2 |
15.4 |
12.6 |
|
Vaginal sex |
38.8 |
48.9 |
32.8 |
44.4 |
Source: La Trobe University, National Survey of Australian Secondary Students and Sexual Health 2018, Table 5.12 Reported sexual behaviours by year level and gender
*Given the substantial sample size, for the first time in addition to female and male, the national survey report includes results for people who identify as trans and gender diverse (TGD). However, the number of responses from TGD participants were too small to be tested statistically.
Just over 50 per cent of young people had given or received oral sex. Young people are giving or receiving oral sex at an earlier age than previous generations.14,15 This has implications for sex education, particularly regarding engaging in safe oral sex with appropriate protection against sexually transmitted infections.
In 2018, Australian Year 10 to Year 12 secondary students who had had sexual intercourse reported on the number of sexual partners they had in the past year.
|
Male |
Female |
Trans and gender diverse** |
Total |
|
|
I have not had sex in the past year |
5.4 |
2.8 |
13.6 |
3.9 |
|
1 person |
59.6 |
63.0 |
40.9 |
61.5 |
|
2 people |
15.5 |
15.5 |
18.2 |
15.5 |
|
3 or more people |
19.4 |
18.7 |
27.3 |
19.0 |
Source: La Trobe University, National Survey of Australian Secondary Students and Sexual Health 2018, Table 5.14 Responses to “Over the last year with how many people have you had anal and/or vaginal intercourse?”
* Defined as young people who have had sexual intercourse.
** Given the substantial sample size, for the first time in addition to female and male, the national survey report includes results for people who identify as trans and gender diverse (TGD). However, the number of responses from TGD participants were too small to be tested statistically.
Female students were slightly more likely than male students to report fewer partners in the previous year.16 The numbers are too small to report statistical differences for the trans and gender diverse students.
Studies have suggested that the early initiation of sexual activity may sometimes be unwanted or pressured.17,18 In the National Survey sexually active Year 10 to Year 12 students were asked if they had ever had unwanted sex.19 Over one-third (36.8%) of sexually active female students have had unwanted sex, compared to 15.9 per cent of sexually active male students.20
Fifty-two (52%) per cent of young people who reported they had unwanted sex said they were influenced by their partner, with similar results for male and female young people, while 34 per cent of male and female young people reported being too drunk. Female young people were more likely to report that they were frightened (32.3% compared to 27.5%), while male young people were more likely to feel pressure from their peers (17.0% compared to 6.6%).21
Female young people are more likely to experience sexual violence in intimate relationships and in the community than male young people. Female young people in WA aged 15 to 19 years have the highest risk of sexual assault22 across all age groups.23,24 The 2016 Personal Safety survey, found that an estimated 17 per cent of all women in Australia have experienced sexual assault in their lifetime (since they were 15 years of age) compared to 4.3 per cent of men.25 For further information refer to the Safe in the community indicator.
There is some evidence to suggest that the increasing availability of pornography has negatively impacted on young people’s intimate relationships.26 In particular, research suggests that frequent or regular viewing of pornography may contribute to young men engaging in coercive behaviours and holding negative views of gender equality.27,28 More research is needed in this area to investigate any relationship between young people’s viewing of pornography and their perspectives on gender equality and/or safe and consensual sex.
Contraception
Almost one-half (46.6%) of young people in Year 10 to Year 12 have had sexual intercourse (vaginal or anal) and a similar prevalence for giving or receiving oral sex, therefore it is important to understand what contraceptive methods, if any, are being used.
|
Total |
|
|
Always used condoms |
38.4 |
|
Often used condoms |
23.8 |
|
Sometimes used condoms |
10.5 |
|
Occasionally used condoms |
14.5 |
|
Never used condoms |
12.8 |
Source: La Trobe University, National Survey of Australian Secondary Students and Sexual Health 2018, Table 5.18 Responses to “When you had sex in the last year, how often were condoms used?”
Only 38.4 per cent of sexually active young people reported always using a condom. This means that 61.6 per cent of sexually active young people are at risk of contracting a sexually transmissible infection.
These results are consistent with a 2018 Australian survey which reported that three quarters (75.1%) of the respondents who were sexually active in the past 12 months engaged at least once in sexual intercourse without using condoms in that time. This included, 69.3 per cent who had sexual intercourse with a regular partner without condoms and 24.1 per cent who had sexual intercourse with a casual partner(s) without condoms.29
Pregnancy is a significant risk for young people who are sexually active. A high proportion of sexually active young people were not using an effective contraceptive method when they last had vaginal sex.
|
Male |
Female |
Trans |
Total |
|
|
Condoms |
54.5 |
53.1 |
30.4 |
53.5 |
|
The pill |
37.7 |
43.5 |
30.4 |
41.0 |
|
Withdrawal |
17.4 |
21.2 |
13.0 |
19.6 |
|
Contraceptive implant |
6.7 |
9.6 |
26.1 |
8.5 |
|
None |
7.2 |
7.8 |
13.0 |
7.6 |
|
Emergency contraception |
3.0 |
4.6 |
8.7 |
4.0 |
|
IUD |
1.6 |
1.4 |
0.0 |
1.5 |
|
Rhythm method |
1.4 |
1.1 |
4.3 |
1.2 |
|
Other |
0.7 |
0.7 |
8.7 |
0.8 |
|
Injection |
0.7 |
0.7 |
0.0 |
0.7 |
|
Diaphragm |
0.3 |
0.1 |
0.0 |
0.2 |
Source: La Trobe University, National Survey of Australian Secondary Students and Sexual Health 2018, Table 5.29 Responses to “The last time you had vaginal sex which, if any, forms of contraception did you or the person you had sex with use to prevent pregnancy?”
* Given the substantial sample size, for the first time in addition to female and male, the national survey report includes results for people who identify as trans and gender diverse (TGD). However, the number of responses from TGD participants were too small to be tested statistically.
Sexually active Year 10 to Year 12 students’ contraceptive method during last sexual encounter, per cent, Australia, 2018
Source: La Trobe University, National Survey of Australian Secondary Students and Sexual Health 2018, Table 5.29 Responses to “The last time you had vaginal sex which, if any, forms of contraception did you or the person you had sex with use to prevent pregnancy”
* Given the substantial sample size, for the first time in addition to female and male, the national survey report includes results for people who identify as trans and gender diverse (TGD). However, the number of responses from TGD participants were too small to be tested statistically.
The three most common contraceptive methods reported were condoms (53.5%), the pill (41.0%), and the withdrawal method (19.6%). A significant proportion of young people (7.6%) also reported they used no contraceptive method during their last sexual encounter. Furthermore, the use of the withdrawal method is known to be an ineffective form of birth control and as many as one in five people get pregnant every year with this form of contraception.30
Aboriginal young people
In SOS19, a slightly greater proportion of Aboriginal than non-Aboriginal Year 9 to 12 students reported that they had had sex (27.9% compared to 23.9%), however this difference was not statistically significant.
|
Aboriginal |
Non-Aboriginal |
|
|
No |
59.2 |
69.6 |
|
Yes |
27.9 |
23.9 |
|
Prefer not to say |
13.0 |
6.5 |
Source: Commissioner for Children and Young People WA 2020, Speaking Out Survey 2019 Data Tables [unpublished]
The Goanna Survey considers sexual health and relationships in young Aboriginal peoples aged 16 to 29 years across Australia.31 The age range for this study means that most of the data is not directly comparable to the results above.
The 2020 survey found that the median age of vaginal sex was 16 years for female and male Aboriginal young people.32 This is slightly lower than for the general population (17 years).
The proportion of Aboriginal young people reporting having had oral, vaginal or anal sex was marginally lower in remote areas (79%), in comparison to metropolitan and regional areas (81% and 83% respectively).33
Less than one-half (47%) of Aboriginal young people aged 16 to 19 years, used a condom in their last sexual encounter.34 Approximately one in five (22%) Aboriginal young people the same age, reported never using a condom when they had sex.35 This is consistent with the 23.3 per cent of sexually active Australian young people who did not use a condom in the past 12 months.36
A very high proportion (91%) of the 16 to 19 year-old respondents reported their last experience of sex was wanted.37
Lesbian, gay, bisexual, trans and intersex young people
Data on the experiences of Lesbian, gay, bisexual, transgender and intersex (LGBTI)38 young people are discussed in the next measure: Sexual health.
Children and young people in the youth justice system
The Banksia Hill Detention Centre is the only facility in WA for the detention of children and young people 10 to 17 years of age who have been remanded or sentenced to custody. During 2019–20, approximately 107 children and young people aged between 10 and 17 years were held in the Banksia Hill Detention Centre in WA on an average day.39
There is evidence to suggest that young people in the youth justice system are at higher risk of STIs,40,41 although there is no data available on the sexual health of young people in detention in WA.
In 2015 the Young People in Custody Health Survey (YPICHS) was conducted in NSW across seven juvenile justice centres. Of the young people invited to participate, 90.4% completed the survey which represented 59.3% of young people in custody at the time across NSW.42
Young people in the youth justice system are more likely to be sexually active than those in the broader population. The majority (96.9%) of the YPICHS participants and 92.2 per cent of the participants under the age of 16 years reported having had either vaginal, anal or oral sex. This is in contrast to around 50.0 per cent of Year 10 to Year 12 students in the broader population having given or received oral sex and 46.6 per cent having had sexual intercourse.43
Two in three (60.8%) of the sexually active young people reported having had more than one sexual partner in the past year.44 There were no significant differences for these results by gender or Aboriginality.
The most common forms of contraception options for young people in custody in NSW was condoms (44.1%) and the implant, Implanon (12.4%). Approximately one-third (34.7%) of young people in the study reported using no contraception.45 Of concern was that just under one in three (27.7%) young people reported having never used a condom; the same proportion of participants reported using condoms all the time.46
Relationships and sexuality education
A significant proportion of WA high school students are sexually active, therefore ensuring young people have a knowledge and understanding of sex and healthy relationships is essential.
In SOS19, most (85.7%) WA Year 7 to Year 12 students reported that they received some sex education as part of their health and physical education subjects. Of concern, is that almost one in ten (8.4%) high school students reported that they had not received any sex education (11.3% of Year 7 to Year 9 students and 5.1% of Year 10 to Year 12 students).
More specifically, 20.0 per cent of Year 7 to Year 12 students reported that they have learnt nothing about pregnancy and contraception at school. This comprises 28.7 per cent of Year 7 to Year 9 students and 10.3 per cent of Year 10 to Year 12 students.
|
Male |
Female |
Metropolitan |
Regional |
Remote |
Total |
|
|
A lot |
26.1 |
25.6 |
25.0 |
27.8 |
30.3 |
25.7 |
|
Some |
33.1 |
30.5 |
30.8 |
36.7 |
33.2 |
31.8 |
|
A little bit |
21.9 |
23.0 |
22.9 |
21.2 |
20.3 |
22.5 |
|
Nothing |
18.9 |
20.9 |
21.2 |
14.2 |
16.3 |
20.0 |
Source: Commissioner for Children and Young People WA 2020, Speaking Out Survey 2019 Data Tables [unpublished]
While gaining an understanding of contraception is critical for young people, understanding safe and healthy relationships more broadly is also essential, including discussions of respectful relationships and consent.
Almost one-third of Year 7 to Year 12 students (31.9%) reported that they have learnt a little bit or nothing about sexual health. Only one-quarter (24.6%) of Year 7 to Year 12 students reported that they have learnt a lot about sexual health.
|
Male |
Female |
Metropolitan |
Regional |
Remote |
Total |
|
|
A lot |
26.8 |
22.5 |
23.2 |
28.7 |
34.2 |
24.6 |
|
Some |
45.7 |
41.4 |
43.5 |
44.7 |
39.8 |
43.5 |
|
A little bit |
18.4 |
25.9 |
22.8 |
18.9 |
19.8 |
22.1 |
|
Nothing |
9.1 |
10.2 |
10.4 |
7.7 |
6.1 |
9.8 |
Source: Commissioner for Children and Young People WA 2020, Speaking Out Survey 2019 Data Tables [unpublished]
Over one-quarter (26.2%) of Year 10 to Year 12 students reported that they had learnt nothing (8.2%) or a little bit (18.0%) about sexual health. Almost one-third (31.9%) reported they had learnt a lot and 42.0 per cent reported they had learnt some.
|
Years 7 to 9 |
Years 10 to 12 |
|
|
A lot |
18.1 |
31.9 |
|
Some |
44.8 |
42.0 |
|
A little bit |
25.8 |
18.0 |
|
Nothing |
11.3 |
8.2 |
Source: Commissioner for Children and Young People WA 2020, Speaking Out Survey 2019 Data Tables [unpublished]
Less than one-half (43.6%) of Year 7 to Year 12 students who had sex education at school said that it was extremely (11.8%) or very (31.8%) relevant. Almost 10 per cent (9.1%) reported that it was not at all relevant and 47.3 per cent said it was somewhat relevant.47
More than one in eight (13.2%) young people in Years 7 to 12 feel like they do not know enough about sexual health, while a similar proportion (13.5%) were not sure. Three-quarters (73.3%) of Year 7 to Year 12 students report that they feel like they know enough about sexual health.
|
Male |
Female |
Metropolitan |
Regional |
Remote |
Total |
|
|
No |
13.3 |
18.6 |
16.3 |
15.6 |
9.7 |
13.2 |
|
Yes |
68.4 |
57.3 |
63.1 |
63.1 |
60.0 |
73.3 |
|
I'm not sure |
18.2 |
24.1 |
20.6 |
21.3 |
30.3 |
13.5 |
Source: Commissioner for Children and Young People WA 2020, Speaking Out Survey 2019 Data Tables [unpublished]
Male students were significantly more likely to say they knew enough about sexual health (68.4% of male students compared to 57.3% of female students). Two in five female students (42.7%) felt that either did not know enough or were not sure compared to 31.5 per cent of male students.
Students in remote locations were significantly more likely than those in regional and metropolitan locations to respond that they were not sure (30.3% in remote locations responded they were not sure compared to 21.3% in regional and 20.6% in metropolitan).
Endnotes
- Victorian Department of Education and Early Childhood Development 2014, Building Respectful Relationships: Stepping out against gender-based violence, Victorian Government, p. 7.
- Australian Institute of Health and Welfare (AIHW) 2011, Young Australians: their health and wellbeing 2011, Cat no PHE 140, AIHW, p. 80.
- Commissioner for Children and Young People WA 2020, Speaking Out Survey: The views of WA children and young people on their wellbeing - a summary report, Commissioner for Children and Young People WA.
- Australian Study of Health and Relationships (ASHR) 2014, Sex in Australia 2 – Summary, The University of NSW, The University of Sydney, University of Sussex and La Trobe University.
- Rissel C et al 2014, First vaginal intercourse and oral sex among a representative sample of Australian adults: the Second Australian Study of Health and Relationships, Sexual Health, Vol 11.
- Ibid, p. 409.
- Fisher CM et al 2019, National Survey of Australian Secondary Students and Sexual Health 2018, ARCSHS Monograph Series No. 113, Australian Research Centre in Sex, Health & Society, La Trobe University, p. 17.
- Ibid, p. 20.
- Ibid, p. 3.
- Mitchell A et al 2014, National Survey of Australian Secondary Students and Sexual Health 2013, Australian Research Centre in Sex, Health and Society, La Trobe University, p. v.
- Fisher CM et al 2019, National Survey of Australian Secondary Students and Sexual Health 2018, ARCSHS Monograph Series No. 113, Australian Research Centre in Sex, Health & Society, La Trobe University, p. 41.
- Ibid, p. 49.
- Ibid, p. 54.
- Australian Study of Health and Relationships (ASHR) 2014, Sex in Australia 2 – Summary, The University of NSW, The University of Sydney, University of Sussex and La Trobe University.
- Rissel C et al 2014, First vaginal intercourse and oral sex among a representative sample of Australian adults: the Second Australian Study of Health and Relationships, Sexual Health, Vol 11, p. 411.
- Fisher CM et al 2019, National Survey of Australian Secondary Students and Sexual Health 2018, ARCSHS Monograph Series No. 113, Australian Research Centre in Sex, Health & Society, La Trobe University, p. 38.
- Wight D et al 2008, The Quality of Young People’s Heterosexual Relationships: A Longitudinal Analysis of Characteristics Shaping Subjective Experience, Perspectives on Sexual Reproductive Health, Vol No 4.
- Dickson N et al 1998, First sexual intercourse: Age, coercion, and later regrets reported by a birth cohort, British Medical Journal, Vol 316, No 7124.
- It should be noted that unwanted sex, is not strictly non-consensual sex. The survey question was: ‘have you ever had sex when you didn’t want to?’. This survey did not ask about non-consensual sex.
- Fisher CM et al 2019, National Survey of Australian Secondary Students and Sexual Health 2018, ARCSHS Monograph Series No. 113, Australian Research Centre in Sex, Health & Society, La Trobe University, p. 39.
- Ibid, p. 39.
- Sexual assault is defined as “an act of a sexual nature carried out against a person’s will through the use of physical force, intimidation or coercion, and includes any attempts to do this. This includes rape, attempted rape, aggravated sexual assault (assault with a weapon), indecent assault, penetration by objects, forced sexual activity that did not end in penetration and attempts to force a person into sexual activity.” Sexual assault excludes unwanted sexual touching which is included in sexual harrassment. Source: ABS, Personal Safety – Methodology glossary [online].
- It should be noted that this data is based on crimes recorded by Police Departments across Australia and therefore will underestimate the prevalence of sexual assault, particularly for young women.
- Australian Bureau of Statistics 2020, 4510.0 - Recorded Crime - Victims, Australia, 2019, Table 7 Victims, Age by selected offences and sex, States and territories, 2019.
- Australian Bureau of Statistics 2017, Personal Safety, Australia: 2016 – Prevalence of violence since age of 15, ABS.
- Australian research in 2010 found that around 60 per cent of young people aged 13 to 16 years had seen sexual images either online or offline in the past 12 months. Green et al 2011, Risks and safety for Australian children on the internet, Cultural Science Journal, Vol 4, No 1, p. 29.
- Stanley N et al 2016, Pornography, Sexual Coercion and Abuse and Sexting in Young People’s Intimate Relationships: A European Study, Journal of Interpersonal Violence, Vol 33, No 19.
- Horvath M et al 2013, “Basically... porn is everywhere” A Rapid Evidence Assessment on the Effect that Access and Exposure to Pornography has on Children and Young People, Office of the Children's Commissioner, p. 7.
- Adam P et al 2019, Sexual health-related knowledge, attitudes and practices of young people in Australia. Results from the 2018 Debrief Survey among heterosexual and non-heterosexual respondents, Centre for Social Research in Health, UNSW Sydney, p. 22.
- Center for Disease Control and Prevention [undated], Effectiveness of Family Planning Methods, US Department of Health and Human Services.
- Just under 1,343 Aboriginal young people aged 16 to 29 years participated in the 2020 survey, with data collection points available at community, sporting and cultural events across Australia between September 2017 and January 2020. Source: Ward J et al 2020, The Goanna Survey 2: Results of the second Australian survey of knowledge, relationships, behaviour and health service access relating to sexually transmissible infections (STIs) and blood borne viruses (BBVs) among Aboriginal and Torres Strait Islander young people, The Kirby Institute, University of New South Wales, p. 9.
- Ibid, p. 22.
- Ibid, p. 24.
- Ibid, p. 31.
- Ibid, p. 31.
- Adam P et al 2019, Sexual health-related knowledge, attitudes and practices of young people in Australia. Results from the 2018 Debrief Survey among heterosexual and non-heterosexual respondents, Centre for Social Research in Health, UNSW Sydney, p. 18.
- Ward J et al 2020, The Goanna Survey 2: Results of the second Australian survey of knowledge, relationships, behaviour and health service access relating to sexually transmissible infections (STIs) and blood borne viruses (BBVs) among Aboriginal and Torres Strait Islander young people, The Kirby Institute, University of New South Wales, p. 34.
- The Commissioner for Children and Young People understands there are a range of terms and definitions that people use to define their gender or sexuality. The Commissioner’s office will use the broad term LGBTI to inclusively refer to all people who are lesbian, gay, bisexual, trans and intersex, as well as to represent other members of the community that use different terms to describe their diverse sexuality and/or gender.
- WA Department of Justice 2020, Annual Report: 2019–20, WA Government, p. 34.
- Belenko S et al, 2008, Recently arrested adolescents are at high risk for sexually transmitted diseases, Sexually transmitted diseases, Vol 35, No 8.
- The Royal Australasian College of Physicians (RACGP) 2011, The health and well-being of incarcerated adolescents, RACGP, p. 32.
- Justice Health & Forensic Mental Health Network and Juvenile Justice NSW 2015, 2015 Young People in Custody Health Survey: Full Report, NSW Government.
- Fisher CM et al 2019, National Survey of Australian Secondary Students and Sexual Health 2018, ARCSHS Monograph Series No. 113, Australian Research Centre in Sex, Health & Society, La Trobe University
- Ibid, p. 53.
- Ibid, p. 54.
- Ibid, p. 54.
- Commissioner for Children and Young People WA 2020, Speaking Out Survey 2019 Data Tables, Commissioner for Children and Young People WA [unpublished].
Last updated August 2021
Good sexual health is important for young people’s physical health and overall wellbeing. Sexual health includes not only safe sex practices to reduce the risk of sexually transmissible infections (STI) and pregnancy, but also appropriate access to information and services that are inclusive and culturally safe. This section focuses on prevalence of STIs in young people in WA to highlight the importance of education programs and services to support young people to live healthy and happy lives.
STIs are most commonly contracted through unsafe sexual practices and can be either bacterial or viral and have serious long term complications if left untreated.1 These consequences include chronic abdominal pain, infertility and genital, heart and brain damage.2 They are often undiagnosed as they can have no symptoms.3
Young people between the ages of 15 and 29 years account for a significant proportion of STI notifications annually.4 The prevention, testing and treatment of young people is a considerable challenge for a variety of reasons including, young people often underestimated the seriousness of STIs, financial costs can be a barrier as can social stigma. This results in many of the cases of STI infection in young people remaining undiagnosed and untreated.5 Young people are particularly vulnerable to STIs due to risk factors such as increased sexual activity, risky alcohol and drug consumption, lack of knowledge about STIs and the prevalence of undiagnosed conditions.6
The most common STIs that are considered a health risk for young people are chlamydia, syphilis and gonorrhoea. These STIs are nationally notifiable diseases. This means state and territory health authorities supply notifications of chlamydia, gonorrhoea and syphilis to the National Notifiable Diseases Surveillance System to collect information relating to diseases of public importance.
Other sexually transmitted conditions include human immunodeficiency virus (HIV), human papillomavirus (HPV), genital herpes (HSV) and hepatitis (A and B). HIV and hepatitis are not very common, HPV rates are reducing significantly due to the recent introduction of the Gardasil® vaccine and while herpes is very common, it is generally not considered a significant health risk.7,8 Therefore, these conditions are not tracked in this measure.
The WA Department of Health Communicable Disease Control Directorate collects notification data of STIs and produces annual and quarterly reports for Western Australia. The data collected highlights that chlamydia was the most common STI to be diagnosed in young people aged 15 to 19 years, with gonorrhoea the second most common.
|
10 to 14 years |
15 to 19 years |
|||
|
Male |
Female |
Male |
Female |
|
|
Chlamydia |
18.2 |
70.6 |
669.9 |
1,911.9 |
|
Gonorrhoea |
4.9 |
31.5 |
195.6 |
298.1 |
|
Infectious syphilis |
1.2 |
6.3 |
24.6 |
43.5 |
Source: WA Department of Health, Epidemiology of STIs and BBVs in Western Australia, Annual Report: 2019 – Appendix, Table 2 Number and age-specific rate of STI notifications by sex, WA, 2019
* Age-specific rate per 100,000 population.
The prevalence of STIs in young people aged 10 to 14 years is understandably low, however any diagnosis in this age group is a significant cause for concern.
Female young people across age groups are much more likely to be diagnosed with chlamydia and more likely to be diagnosed with gonorrhoea. Rates of infectious syphilis were similar between male and female young people.
Data for WA young people aged 12 to 17 years shows that there has been a significant decrease in the rate of chlamydia notifications since 2012, and an increase in the rate of syphilis notifications. Gonorrhoea notifications had decreased until an increase in 2017.
|
Chlamydia |
Gonorrhoea |
Infectious syphilis |
||||
|
10 to 14 years |
15 to 19 years |
10 to 14 years |
15 to 19 years |
10 to 14 years |
15 to 19 years |
|
|
2012 |
91.7 |
1,932.6 |
51.1 |
350.0 |
- |
1.3 |
|
2013 |
101.8 |
1,854.8 |
48.3 |
326.5 |
- |
2.0 |
|
2014 |
96.2 |
1,652.4 |
44.2 |
252.0 |
- |
6.3 |
|
2015 |
65.5 |
1,509.8 |
34.1 |
224.8 |
0.7 |
8.1 |
|
2016 |
66.3 |
1,473.6 |
52.0 |
334.7 |
1.3 |
11.7 |
|
2017 |
65.0 |
1,442.9 |
38.5 |
352.9 |
2.5 |
23.2 |
|
2018 |
54.4 |
1,367.3 |
21.3 |
233.9 |
0.6 |
21.3 |
|
2019 |
44.0 |
1,272.5 |
18.0 |
247.2 |
3.7 |
33.8 |
Source: WA Department of Health, Epidemiology of STIs and BBVs in Western Australia, Annual Report: 2019 – Appendix (and previous years)
* Age-specific rate per 100,000 population.
Note: This data has been sourced from individual Annual Reports and therefore has not been adjusted for changes in the age and sex structure of the population across these years. No modelling or analysis has been carried out to determine if there is a trend component to the data.
Rate of STI notifications for young people aged 15 to 19 years, age-specific rate, WA, 2012 to 2019
Source: WA Department of Health, Epidemiology of STIs and BBVs in Western Australia, Annual Report: 2019 – Appendix (and previous years)
The WA Department of Health suggest that the reduction in chlamydia notifications for the whole population from 2016 may largely be due to decreased disease transmission.9 Similarly, for gonorrhoea, testing rates have increased in recent years and test positivity rates have decreased, suggesting a decrease in disease transmission.10
Infectious syphilis notifications increased substantially in the whole WA population from 2012 to 2019.11 This is principally due to an outbreak of infectious syphilis affecting young Aboriginal people between 15 and 29 years across Australia.12 It is important to emphasise that a significant proportion of these notifications are as a result of sexual activity with same-aged peers and not due to an increase in child sexual abuse.13
Researchers indicate that this outbreak is influenced by resistance to some antibiotics, poor accessibility to sexual health services in remote areas, high health staff turnover and shortages in Aboriginal health practitioners in these areas.14,15 Infectious syphilis is “fully curable with a single injection of long-acting penicillin”.16
For more information on the syphilis outbreak across Australia refer to the Department of Health’s website.
STI notification rates are generally higher in remote areas across Australia,17 and WA is no exception. In 2019, the Kimberley had a consistently higher rate of notifications across the population for all STIs.
The following data reports the number and rate of notifications of STIs for WA young people aged 15 to 19 years in 2019 by region.
|
Chlamydia |
Gonorrhoea |
Infectious Syphilis |
||||
|
Number |
Rate |
Number |
Rate |
Number |
Rate |
|
|
Goldfields |
61 |
1,731.5 |
26 |
738.0 |
0 |
0.0 |
|
Great Southern |
39 |
982.9 |
3 |
75.6 |
0 |
0.0 |
|
Kimberley |
176 |
7,963.8 |
102 |
4,615.4 |
17 |
769.2 |
|
Metropolitan |
1,500 |
1,118.6 |
179 |
133.5 |
8 |
6.0 |
|
Midwest |
61 |
1,453.8 |
20 |
476.6 |
0 |
0.0 |
|
Pilbara |
94 |
4,164.8 |
64 |
2,835.6 |
27 |
1,196.3 |
|
South West |
140 |
1,197.0 |
10 |
85.5 |
0 |
0.0 |
|
Wheatbelt |
37 |
946.5 |
5 |
127.9 |
1 |
25.6 |
|
Total |
2,111 |
1,272.5 |
410 |
247.2 |
56 |
33.8 |
Source: WA Department of Health 2020, Epidemiology of STIs and BBVs in Western Australia, Annual Report: 2018 – Appendix
* Age-specific rate per 100,000 population.
The above data highlights that the Kimberley has a proportionally very high rate of STI notifications, considering the much smaller population.
Aboriginal young people across Australia are disproportionally impacted by STIs in comparison to non-Aboriginal young people. Thirty two per cent (32.1%) of all notifications for 15 to 19 year-olds in 2019 were for Aboriginal young people, of whom one-third (33.7%) were in the Kimberley.18
The high rate of STIs within the Aboriginal population can be attributed to many factors, which include limited access to high quality and culturally safe health care services, poor sexual health education and living in areas where STIs are more common.19
The Aboriginal Surveillance Report on HIV, viral hepatitis and STIs is an annual report that collates, monitors and reports on patterns of HIV, viral hepatitis and STIs in Australia. The 2018 report provides data on 2017.
|
0 to 14 years |
15 to 19 years |
|||
|
Male |
Female |
Male |
Female |
|
|
Chlamydia |
44.7 |
262.3 |
3,438.8 |
7,450.0 |
|
Gonorrhoea |
22.4 |
162.6 |
1,809.8 |
2,706.2 |
|
Infectious syphilis |
3.1 |
15.3 |
138.1 |
238.0 |
Source: The Kirby Institute, Aboriginal Surveillance Report on HIV, viral hepatitis and STIs 2018, Blood borne viral and sexually transmissible infections in Aboriginal and Torres Strait Islander people
* Rate is per 100,000 population
|
Aboriginal |
Non-Aboriginal |
|||
|
Male |
Female |
Male |
Female |
|
|
Chlamydia |
3,438.8 |
7,450.0 |
649.2 |
1,958.8 |
|
Gonorrhoea |
1,809.8 |
2,706.2 |
95.3 |
105.3 |
|
Infectious syphilis |
138.1 |
238.0 |
10.0 |
3.5 |
Source: The Kirby Institute, Aboriginal Surveillance Report on HIV, viral hepatitis and STIs 2018, Blood borne viral and sexually transmissible infections in Aboriginal and Torres Strait Islander people
* Rate is per 100,000 population
STI notification rate for young people aged 15 to 19 years by Aboriginal status and gender, rate, Australia, 2017
Source: The Kirby Institute, Aboriginal Surveillance Report on HIV, viral hepatitis and STIs 2018, Blood borne viral and sexually transmissible infections in Aboriginal and Torres Strait Islander people
Across Australia, female Aboriginal young people have a significantly higher rate of notifications for chlamydia, gonorrhoea and syphilis. This pattern is similar for female non-Aboriginal young people, who are more likely to have notifications for chlamydia and gonorrhoea than male non-Aboriginal young people. However, male non-Aboriginal young people have a higher rate of syphilis notifications than female non-Aboriginal young people. This is principally because in the metropolitan area there is a higher rate of syphilis among young gay men, while in regional and remote Australia the outbreak of syphilis is mainly affecting heterosexual Aboriginal young people.20
Lesbian, gay, bisexual, trans and intersex young people
Lesbian, gay, bisexual, transgender and intersex (LGBTI)21 young people are at an increased risk of a range of sexual health problems, in particular sexually transmitted infections (STIs).22
LGBTI young people are at a higher risk of contracting an STI for a variety of reasons including lower condom use and higher likelihood of risky alcohol and drug-taking behaviour which can lead to risk-taking sexual activities.23,24
In the 2010 Writing Themselves in 3 (WTi3) survey, 3,134 Australian LGBTI young people aged 14 to 21 years old completed an online questionnaire with both quantitative and qualitative questions regarding their sexual health and wellbeing.25 Due to the ‘opt-in’ nature of this survey, it cannot be considered representative of LGBTI young people, however it provides an indication of LGBTI young people’s sexual experiences.
The survey found that young people identifying as LGBTI were sexually active earlier than their heterosexual peers, however approximately one in three (28%) LGBTI respondents aged 14 to 21 years that participated in the survey had never had sex.26 Female LGBTI young people were marginally more likely to have had sex than their male counterparts (74.0% compared to 69.0%).27
Just under half (45%) of the LGBTI young people aged 15 to 18 years who had had sexual intercourse (vaginal or anal) reported using a condom when they last had sexual intercourse.28 This is low compared to the general population with 59 per cent of sexually active secondary students reporting using a condom.29
It should be noted that the Writing themselves In 4 report was released in February 2021, however the 2019 survey did not ask LGBTI young people about their sexual experiences.30
In 2018, the Kirby Institute conducted the first sexual health survey with 1,613 trans and gender diverse Australians.31 The survey found that trans and gender diverse people reported experiencing very high rates of marginalisation in sexual health care and this was associated with lower testing rates for STIs than in the broader population. Trans and gender-diverse Australians also reported inconsistent condom use with casual partners.32 While these results are not specifically for young people, they highlight how important it is for information at schools and at health services to be inclusive and supportive of trans and gender diverse young people.
There is no other data on the experience of sexual health issues by WA young people who identify as LGBTI.
For more information on LGBTI children and young people, refer to the Commissioner’s issues paper:
Commissioner for Children and Young People WA 2018, Lesbian, Gay, Bisexual, Trans and Intersex (LGBTI) children and young people, Commissioner for Children and Young People WA
Culturally and linguistically diverse young people
Data and research suggests that people from culturally and linguistically diverse (CALD) backgrounds often have low sexual health literacy, which means that they are less likely to access the services that they need, experience social isolation, and have lower levels of knowledge and understanding of sexual health issues.33
Some young people from CALD backgrounds (and their families) experience language barriers, feeling torn between cultures, intergenerational conflict, racism and discrimination, bullying and resettlement stress.34 Some of these young people have traumatic pre-migration experiences, including family separation, war, violence and immigration detention, which can also impact their mental health and wellbeing.
Through either migration or forced resettlement, many CALD and refugee young people may have experienced a disruption to their education, reduced access to health care and family and social disruptions.35 In addition, current sexual health education and sexual health services may be discriminatory or exclusive, and reduce the possibility of CALD and refugee young people feeling comfortable to ask questions, and seek help or advice.36,37
There is no data available on the sexual health of young people in WA of a CALD background.
For more information on children and young people from culturally and linguistically diverse backgrounds in WA, refer to the Commissioner’s policy brief:
Commissioner for Children and Young People WA 2013, The mental health and wellbeing of children and young people: Children and Young People from Culturally and Linguistically Diverse Backgrounds, Commissioner for Children and Young People WA.
Children and young people in the youth justice system
The Banksia Hill Detention Centre is the only facility in WA for the detention of children and young people 10 to 17 years of age who have been remanded or sentenced to custody. During 2019–20, approximately 107 children and young people aged between 10 and 17 years were held in the Banksia Hill Detention Centre in WA on an average day.38
International research suggests adult custodial settings may be high-risk environments for the transmission of STIs.39 There is some evidence that this may also be the case in juvenile detention centres,40,41 although there is no data available on the sexual health of young people in detention in WA.
In 2015 the Young People in Custody Health Survey (YPICHS) was conducted in NSW across seven juvenile justice centres. Of the young people invited to participate, 90.4% completed the survey which represented 59.3% of young people in custody at the time across NSW.42
This study found that one in ten (10.1%) young people in custody had been diagnosed with an STI in the past, with chlamydia the most common (9.6%).43
Endnotes
- Australian Bureau of Statistics 2012, Australian Social Trends: June 2012 – Sexually transmissible infections, ABS.
- Ibid.
- Ibid.
- Department of Health 2018, Fourth National Sexually Transmissible Infections Strategy 2018–2022, Australian Government.
- Ibid, p. 20.
- Ibid, p. 20.
- Australian Bureau of Statistics 2012, Australian Social Trends: June 2012 – Sexually transmissible infections, ABS.
- Department of Health 2018, Fourth National Sexually Transmissible Infections Strategy 2018–2022, Australian Government.
- WA Department of Health, Epidemiology of STIs and BBVs in Western Australia, Annual Report: 2019, WA Government, p. 15.
- Ibid, p. 21.
- Ibid, p. 21.
- Department of Health 2020, Infectious syphilis outbreak, Australian Government [website].
- Ward J et al 2015, Northern Australia syphilis outbreak is about government neglect, not child abuse, The Conversation [website].
- Ibid.
- Kirby Institute 2018, Bloodborne viral and sexually transmissible infections in Aboriginal and Torres Strait Islander people: annual surveillance report 2018, Kirby Institute, UNSW Sydney, p. 9.
- Ibid, p. 103.
- Kirby Institute 2017, HIV, viral hepatitis and sexually transmissible infections in Australia: annual surveillance report 2017, Kirby Institute, UNSW Sydney, p. 124, 142 and 159.
- Calculated by Commissioner for Children and Young People WA from WA Department of Health 2020, Epidemiology of STIs and BBVs in Western Australia, Annual Report: 2018 – Appendix
- Australian Institute of Health and Welfare (AIHW) 2013, Demonstration projects for improving sexual health in Aboriginal and Torres Strait Islander youth: Evaluation report, Cat no IHW 81, AIHW
- Department of Health 2018, Fourth National Sexually Transmissible Infections Strategy 2018–2022, Australian Government, p. 15.
- The Commissioner for Children and Young People understands there are a range of terms and definitions that people use to define their gender or sexuality. The Commissioner’s office will use the broad term LGBTI to inclusively refer to all people who are lesbian, gay, bisexual, trans and intersex, as well as to represent other members of the community that use different terms to describe their diverse sexuality and/or gender.
- Hillier L et al 2010, Writing Themselves in 3: The third national study on the sexual health and wellbeing of same sex attracted and gender questioning young people, Australian Research Centre in Sex, Health and Society, La Trobe University, p. ix.
- Hegazi A and Pakianathan M 2018, LGBT Sexual Health, Medicine, Vol 46, No 5.
- Hillier L et al 2010, Writing Themselves in 3: The third national study on the sexual health and wellbeing of same sex attracted and gender questioning young people, Australian Research Centre in Sex, Health and Society, La Trobe University, p. 35.
- Hillier L et al 2010, Writing Themselves in 3: The third national study on the sexual health and wellbeing of same sex attracted and gender questioning young people, Australian Research Centre in Sex, Health and Society, La Trobe University, p. ix.
- Ibid, p. 33.
- Ibid, p. 33.
- Ibid, p. 34.
- Mitchell A et al 2014, 5th National Survey of Australian Secondary Students and Sexual Health 2013, Australian Research Centre in Sex, Health and Society, La Trobe University, p. 35.
- Hill A et al 2021, Writing Themselves In 4: The health and wellbeing of LGBTQA+ young people in Australia - National report, La Trobe University.
- Callander D et al 2019, The 2018 Australian Trans and Gender Diverse Sexual Health Survey: Report of Findings, The Kirby Institute.
- Ibid, p. 12 and 14.
- Ethnic Communities Council of Victoria 2013, Sexual Health, Cultural Diversity and Young People: What Do We Know?, Ethnic Communities Council of Victoria, p. 3.
- WA Office of Multicultural Interests 2009, Not drowning, waving: Culturally and linguistically diverse young people at risk in Western Australia, WA Government, p. 5.
- Claudine Ngum Chi Watts M et al 2015, Factors Influencing Contraception Awareness and Use: The Experiences of Young African Australian mothers, Journal of Refugee Studies, Vol 28, No 3.
- Brown G et al 2011, How they got it and how they wanted it: Marginalised young people's perspective on their experiences of sexual health education, Sex Education, Vol 12, No 5.
- Mengesha ZB et al 2016, Culturally and linguistically diverse women’s views and experiences of accessing sexual and reproductive health care in Australia: a systematic review, Sexual Health, Vol 13, No 4.
- WA Department of Justice 2020, Annual Report: 2019–20, WA Government, p. 34.
- Department of Health 2018, Fourth National Sexually Transmissible Infections Strategy 2018-2022, Australian Government, p. 23.
- Belenko S et al, 2008, Recently arrested adolescents are at high risk for sexually transmitted diseases, Sexually transmitted diseases, Vol 35, No 8.
- The Royal Australasian College of Physicians (RACGP) 2011, The health and well-being of incarcerated adolescents, RACGP, p. 32.
- Justice Health & Forensic Mental Health Network and Juvenile Justice NSW 2015, 2015 Young People in Custody Health Survey: Full Report, NSW Government.
- Ibid, p. 54.
Last updated August 2021
Births to teenage mothers1 are associated with a higher likelihood of adverse health, education and economic outcomes for both mother and baby. Parenthood during the teenage years often means that the mother’s education is interrupted, her future job prospects are limited, and there is a higher likelihood that she will be more dependent on government assistance over her lifetime.2,3
Babies of teenage mothers are at a greater risk of low birth weight and pre-term birth.4 This can be due to the age of the mother, but also reflects certain risk factors which are more prevalent among teenage mothers, including socioeconomic disadvantage and a higher likelihood of smoking during pregnancy.5,6 Teenage mothers are also less likely to attend antenatal care, which can be a protective factor against these risks.7
The Australian Bureau of Statistics (ABS) collects all birth registrations within Australia each year; this data does not include stillbirths or foetal deaths. This data is used to calculate fertility rates per 1,000 women by age.
|
15 years |
16 years |
17 years |
18 years |
19 years |
15 to 19 years |
|
|
2006 |
3.2 |
8.7 |
18.1 |
28.7 |
40.5 |
19.8 |
|
2007 |
4.6 |
9.6 |
19.1 |
28.8 |
40.4 |
20.6 |
|
2008 |
4.2 |
11.7 |
19.1 |
30.4 |
46.9 |
22.8 |
|
2009 |
4.9 |
8.2 |
19.1 |
26.9 |
40.0 |
20.2 |
|
2010 |
4.8 |
8.3 |
15.5 |
28.5 |
38.1 |
19.3 |
|
2011 |
3.8 |
8.6 |
16.4 |
26.6 |
40.6 |
19.4 |
|
2012 |
3.9 |
7.5 |
17.7 |
25.7 |
37.1 |
18.6 |
|
2013 |
3.9 |
7.5 |
15.9 |
22.2 |
36.2 |
17.4 |
|
2014 |
3.5 |
6.0 |
12.8 |
21.5 |
33.0 |
15.6 |
|
2015 |
2.8 |
7.2 |
12.6 |
19.0 |
31.3 |
14.7 |
|
2016 |
3.6 |
6.2 |
11.2 |
17.3 |
27.7 |
13.3 |
|
2017 |
2.9 |
5.7 |
9.6 |
16.4 |
28.0 |
12.6 |
|
2018 |
2.1 |
3.9 |
7.6 |
13.7 |
22.6 |
10.2 |
|
2019 |
1.7 |
3.9 |
7.9 |
12.7 |
21.9 |
9.8 |
Source: Australian Bureau of Statistics, ABS.Stat: Fertility rates by age, by state for Western Australia
* Age-specific fertility rates are the number of live births (registered) during the calendar year, according to the age of the mother, per 1,000 of the female estimated resident population of the same age at 30 June.
Fertility rates for female young people aged 15 to 19 years, age-specific rate, WA, 2006 to 2019
Source: Australian Bureau of Statistics, ABS.Stat: Fertility rates by age, by state for Western Australia
While, the rate of births to WA female young people aged 15 to 19 years has decreased steadily over the last decade, these rates are higher than the Australian fertility rates for these ages.
|
WA |
Australia |
|
|
15 years |
1.7 |
1.3 |
|
16 years |
3.9 |
3.0 |
|
17 years |
7.9 |
6.4 |
|
18 years |
12.7 |
11.6 |
|
19 years |
21.9 |
19.7 |
|
15 - 19 years |
9.8 |
8.7 |
Source: Australian Bureau of Statistics, ABS.Stat: Fertility rates by age, by state
In 2019, there were 200 births to young mothers under the age of 18 years across WA. This included, 25 births to mothers aged 15 years and under, 58 births to mothers aged 16 years and 117 births to mothers aged 17 years. This is a reduction on previous years.
|
2016 |
2017 |
2018 |
2019 |
|
|
15* |
53 |
42 |
31 |
25 |
|
16 |
94 |
85 |
58 |
58 |
|
17 |
168 |
146 |
114 |
117 |
|
Under 18 years |
315 |
273 |
203 |
200 |
Source: Australian Bureau of Statistics, ABS.Stat: Births by age, by state
* Includes births to mothers under 15 years of age.
Across Australia, teenage pregnancies are generally more common in remote and regional areas.8 This is consistent with the data from WA.
|
2015 |
2016 |
2017 |
2018 |
2019 |
|
|
Major cities |
11.2 |
10.0 |
9.4 |
8.4 |
7.4 |
|
Inner regional |
16.5 |
15.4 |
13.7 |
11.7 |
10.2 |
|
Outer regional |
28.7 |
25.4 |
23.4 |
20.2 |
18.1 |
|
Remote |
41.4 |
38.1 |
34.5 |
30.0 |
31.0 |
|
Very remote |
75.6 |
74.7 |
76.0 |
72.5 |
68.6 |
Source: ABS, Births Australia 2019, Births, Summary, Remoteness Areas (ASGS 2016) – 2012 to 2019
Age-specific fertility rate for mothers aged 15 to 19 years by remoteness area, age-specific rate per 1,000 women, WA, 2015 to 2019
Source: ABS, Births Australia 2019, Births, Summary, Remoteness Areas (ASGS 2016) –2012 to 2019
Research suggests this may be influenced by lower access to health services and sexual health education, limited access to abortion, lower education levels and reduced employment opportunities.9,10 Aboriginal female young people are more likely to have a child while under the age of 18 years, than non-Aboriginal female young people.
|
Aboriginal |
Non-Aboriginal |
Total |
|
|
1994 |
151.4 |
20.3 |
26.0 |
|
1995 |
133.6 |
19.8 |
24.7 |
|
1996 |
125.9 |
19.6 |
24.4 |
|
1997 |
135.4 |
17.8 |
23.1 |
|
1998 |
130.6 |
18.8 |
24.0 |
|
1999 |
125.2 |
18.4 |
23.4 |
|
2000 |
122.6 |
17.2 |
22.2 |
|
2001 |
104.1 |
16.3 |
20.9 |
|
2002 |
101.0 |
16.4 |
20.9 |
|
2003 |
100.1 |
14.6 |
19.3 |
|
2004 |
97.8 |
15.3 |
19.9 |
|
2005 |
107.0 |
15.9 |
21.2 |
|
2006 |
105.0 |
16.4 |
21.5 |
|
2007 |
94.1 |
16.5 |
20.9 |
|
2008 |
93.4 |
16.3 |
20.7 |
|
2009 |
88.0 |
15.4 |
19.6 |
|
2010 |
81.4 |
14.1 |
18.0 |
|
2011 |
83.2 |
14.1 |
18.2 |
|
2012 |
77.6 |
13.9 |
17.6 |
|
2013 |
78.3 |
12.1 |
16.1 |
|
2014 |
68.1 |
10.5 |
13.9 |
|
2015 |
58.6 |
9.5 |
12.5 |
Source: WA Department of Health, Mothers and Babies, Western Australia, Western Australia’s mothers and babies 2015
* Age-specific birth rate was calculated from the total number of births in one year per 1,000 women of the same age group.
Birth rates and Aboriginal status for young women aged under 19 years who gave birth in WA, age-specific rate per 1,000 women, WA, 1994 to 2015
Source: WA Department of Health, Mothers and Babies, Western Australia, Western Australia’s mothers and babies 2015
Birth rates for Aboriginal and non-Aboriginal young mothers aged 15 to 19 years in WA have been decreasing over the last 20 years. The birth rate for Aboriginal young mothers has significantly reduced from 151.4 to 58.6 per 1,000 women. Nevertheless, a significantly higher proportion of young Aboriginal women and girls in WA than non-Aboriginal women and girls are still having children as teenagers.
In 2015, teenagers accounted for 16.2 per cent of Aboriginal women who gave birth. In comparison, teenage births accounted for 2.1 per cent of non-Aboriginal women who gave birth.11
Aboriginal female young people have a higher likelihood of becoming mothers at an earlier age than non-Aboriginal female young people for a number of reasons, including: living in remote and regional locations, greater likelihood of socioeconomic disadvantage, less access to health services and lower education levels.12,13
At the same time, research has found that some female Aboriginal young people felt that having children was an opportunity to transform their lives, with a strong desire to be a good parent.14,15
For more information on pregnancy care for young Aboriginal mothers refer to:
Reibel T and Morrison L 2014, Young Aboriginal Women’s Voices on Pregnancy Care, Telethon Kids Institute, The University of Western Australia.
While data and research often focuses on teenage mothers, male young people who become teenage fathers are also important. Similar to teenage mothers, evidence suggests that teenage fathers are more likely to come from socioeconomically disadvantaged backgrounds, single parent families and have lower education levels.16
|
15 years |
16 years |
17 years |
18 years |
19 years |
|
|
2006 |
1.0 |
1.2 |
4.9 |
9.2 |
16.7 |
|
2007 |
0.7 |
2.2 |
5.0 |
10.0 |
15.5 |
|
2008 |
0.9 |
2.1 |
6.1 |
12.1 |
16.5 |
|
2009 |
0.8 |
2.9 |
4.7 |
10.6 |
16.5 |
|
2010 |
0.8 |
1.7 |
5.8 |
9.0 |
15.8 |
|
2011 |
0.7 |
1.7 |
5.7 |
9.6 |
15.2 |
|
2012 |
0.8 |
2.0 |
4.5 |
8.8 |
15.1 |
|
2013 |
1.0 |
2.4 |
4.8 |
9.2 |
13.0 |
|
2014 |
1.0 |
1.6 |
4.4 |
7.9 |
11.9 |
|
2015 |
0.7 |
1.7 |
4.3 |
8.2 |
11.6 |
|
2016 |
0.5 |
1.5 |
3.8 |
6.8 |
11.7 |
|
2017 |
0.6 |
2.4 |
3.2 |
6.2 |
12.0 |
|
2018 |
0.8 |
1.3 |
2.7 |
4.9 |
8.7 |
|
2019 |
0.4 |
1.3 |
3.4 |
5.8 |
9.1 |
Source: Australian Bureau of Statistics, ABS.Stat: Paternity by age, by state
* This data is not complete as it excludes births where paternity was not acknowledged or where the age of the father is not known.
Paternity rate for male young people aged 15 to 19 years, age-specific rate, WA, 2006 to 2019
Source: Australian Bureau of Statistics, ABS.Stat: Paternity by age, by state
Similar to rates of teenage pregnancy, the rate of WA male young people aged 15 to 19 years fathering children has steadily decreased since 2008 with a slight increase in 2019 for male young people aged 17 to 19 years.
It should be noted that this data is not complete as it only includes births where paternity was acknowledged and the age of the father was recorded.
While it is often assumed that teenage mothers are no longer in a relationship with the father of their child, this is often not the case. Although there is no administrative data available, research suggests that teenage mothers can often be in an ongoing relationship with the father of their child.17,18 It is therefore important, where appropriate, to support teenage fathers (and fathers of children of teenage mothers) to be caring and responsible parents.19
The reduction in teenage birth rates has been linked not only to an increase in availability of effective forms of contraception, but also abortion accessibility across Australia.20,21 In WA, abortions performed before 20 weeks gestation are legal and non-surgical abortions have recently been introduced within Australia.22 Yet, data from the WA Department of Health highlights that the rate of induced abortions have decreased by more than one-half from 2005 to 2018 for young women less than 19 years.
|
15-19 years |
All ages |
|
|
2005 |
21.2 |
18.2 |
|
2006 |
23.6 |
19.2 |
|
2007 |
22.9 |
18.9 |
|
2008 |
22.3 |
18.8 |
|
2009 |
21.3 |
18.7 |
|
2010 |
18.9 |
17.4 |
|
2011 |
18.0 |
17.5 |
|
2012 |
14.7 |
16.3 |
|
2013 |
13.8 |
15.9 |
|
2014 |
11.7 |
15.7 |
|
2015 |
9.1 |
15.0 |
|
2016 |
8.4 |
14.7 |
|
2017 |
7.5 |
14.4 |
|
2018 |
8.1 |
14.3 |
Source: WA Department of Health, Reports on induced abortions in Western Australia, Induced Abortions in Western Australia, 2016-2018: Report of the WA Abortion Notification System
Abortion rate by age group, rate,* WA, 2005 to 2018
Source: WA Department of Health, Reports on induced abortions in Western Australia, Induced Abortions in Western Australia, 2016-2018: Report of the WA Abortion Notification System
* Rate per 1,000 women
The abortion rate for WA female young people has steadily decreased from 21.2 per 1,000 women aged 15 to 19 years in 2005 to 8.1 per 1,000 women aged 15 to 19 years in 2018. In 2018 there were 23 abortions across the state for female young people aged under 15 years, this is a significant reduction from 37 in 2005.
Aboriginal female young people in WA aged 15 to 19 years are less likely to have an abortion when pregnant than non-Aboriginal female young people of the same age group.23
The combined reduction in teenage births as well as induced abortions suggests that young people are more effectively using the various contraception options available and that the increase in the quality and accessibility of sexual health education is having an impact.
Endnotes
- In keeping with the terminology used by the Australian Bureau of Statistics and other states, in assessing this measure ‘teen’ and ‘teenage’ are used to indicate persons aged under 19 years of age. Where this measure is highlighting births to mothers aged 17 years and under, that is specifically stated.
- Marino JL et al 2016, Teenage Mothers, Australian Family Physician, Vol 45, No 10.
- Department of Social Services 2016, Try Test Learn Fund: Young Parents Fact Sheet, Australian Government.
- Marino JL et al 2016, Teenage Mothers, Australian Family Physician, Vol 45, No 10.
- Gaudie J et al 2010, Antecedents of teenage pregnancy from a 14-year follow-up study using data linkage, BMC Public Health, Vol 10, No 63.
- Australian Institute of Health and Welfare (AIHW) 2015, Teenage mothers in Australia in 2015, AIHW.
- Australian Institute of Health and Welfare (AIHW) 2012, A picture of Australia’s children 2012, Cat No PHE 167, AIHW, p. 50.
- Hoffman H and Vidal S 2017, Supporting Teen Families: An Assessment of Youth Childbearing in Australia and Early Interventions to Improve Education Outcomes of Young Parents, Life Course centre: Institute for Social Science Research, The University of Queensland, p. 6.
- Ibid.
- Australian Institute of Health and Welfare (AIHW) 2018, Teenage mothers in Australia in 2015, AIHW.
- WA Department of Health, Western Australia’s mothers and babies report: 2015, p. 37.
- Australian Institute of Health and Welfare (AIHW) 2018, Teenage mothers in Australia 2015, AIHW.
- Hoffman H and Vidal S 2017, Supporting Teen Families: An Assessment of Youth Childbearing in Australia and Early Interventions to Improve Education Outcomes of Young Parents, Life Course centre: Institute for Social Science Research, The University of Queensland, p. 7.
- Ibid.
- Larkins et al 2011, The transformative potential of young motherhood for disadvantaged Aboriginal and Torres Strait Islander women in Townsville, Australia, The Medical Journal of Australia, Vol 194, No 10.
- Olajide N et al 2019, The antecedents and consequences of adolescent fatherhood: A systematic review, Social Science & Medicine, Vol 232.
- Manning W and Cohen J 2015, Teenage Cohabitation, Marriage, and Childbearing, Population research and policy review, Vol 34, No 2.
- Kumar N et al 2018, Adolescent Mothers’ Relationships with their Mothers and their Babies’ Fathers during Pregnancy and Postpartum, Journal of Child and Family Studies, Vol 27.
- Wilkes L et al 2012, ‘I am going to be a dad’: experiences and expectations of adolescent and young adult expectant fathers, Journal of Clinical Nursing, Vol 21.
- Family Planning Victoria, Teenage Pregnancy [website].
- Marino JL and Sawyer S 2019, Monitoring the missing half: why reporting adolescent births is insufficient, The Medical Journal of Australia, Vol 210, No 5.
- de Moel-Mandel C and Shelley J 2017, The legal and non-legal barriers to abortion access in Australia: a review of the evidence, The European Journal of Contraception and Reproductive Healthcare, Vol 22, No 2.
- WA Department of Health 2018, Induced Abortions in Western Australia, 2013-2015, p. 28.
Last updated August 2021
At 30 June 2021, there were 1,902 WA young people in care aged between 12 and 17 years, more than one-half of whom (54.0%) were Aboriginal.1
Family relationships, parenting and the environment that a young person grows up in informs their understanding of how to make responsible choices about alcohol, tobacco and other drug use and sexual activities.2,3 Young people in out-of-home care have generally experienced significant adverse events on an ongoing basis. These may include neglect, food scarcity and physical, sexual and/or emotional abuse. Furthermore, young people in the child protection system have often not had stable and positive adult support to provide advice and information on sex and sexual health.4
These experiences increase the likelihood of these young people engaging in risk-taking behaviours, including risky level of alcohol, tobacco and other drug use and risky sexual activities.5,6,7 Furthermore, young people who have experienced high levels of childhood stress are more likely to experience poor health outcomes, including alcoholism, as adults.8
In a 2016 report research, Anglicare Victoria highlighted that young people in care are more likely than their peers in the broader community to smoke and use illicit drugs.9 Just under three in ten (26.6%) young people in care reported ever having smoked cigarettes, in comparison to one in twenty (5%) young people in the broader community.10 In addition, more than three in ten (33.3%) young people had used an illicit substance in the past 12 months in comparison to 17.6 per cent of the young people in the rest of the community.11
Studies have also shown that young people in care often have received limited formal sexual health education and are more likely to have experienced dysfunctional family relationships.12 This increases their risk of early sexual activity and consequently they have a higher risk of pregnancy and contracting sexually transmissible infections.13
Young people in care are also at greater risk of sexual abuse and assault. The Royal Commission into Institutional Responses to Child Sexual Abuse (the Royal Commission) found that sexual abuse by carers, their family members, visitors, caseworkers and other children and young people in care continues to occur, and that sexual exploitation is a growing concern, especially for children and young people in residential care.14 The Royal Commission identified persistent weaknesses and systemic failures that continue to place children and young people in care at risk of sexual abuse.15
Research shows that young women who have been in care have a higher risk of teenage pregnancy than other young women in Australia.16,17 There is also evidence to suggest that pregnant female young people with a care experience are more reluctant to use health services in the fear that their child may being taken into the child protection system.18
Even though young people in care have higher risk profiles for sexually transmissible infections (early sexual initiation, risk-taking behavior, substance abuse), no data is available on the prevalence of sexually transmissible infections for these young people.
No data exists for WA young people in care regarding their alcohol, tobacco or drug use or their sexual health.
Endnotes
- Department of Communities 2021, Custom report provided by Department of Communities, WA Government [unpublished].
- Potter M and Font S 2019, Parenting influences on adolescent sexual risk-taking: Differences by child welfare placement status, Children and Youth Services Review, Vol 96, p. 135.
- Ibid, p. 134.
- Mendes P 2009, Improving outcomes for teenage pregnancy and early parenthood for young people in out-of-home care, Youth Studies Australia, Vol 28 No 4, p. 13
- Research in practice 2016, Risk-taking adolescents and child protection, Research in practice.
- Potter M and Font S 2019, Parenting influences on adolescent sexual risk-taking: Differences by child welfare placement status, Children and Youth Services Review, Vol 96.
- Somers C et al 2016, Adolescent Girls in Out-of-Home Care: Associations Between Substance Use and Sexual Risk Behavior, Journal of Child & Adolescent Substance Abuse, Vol 25, No 5.
- Franke H 2014, Toxic Stress: Effects, Prevention and Treatment, Children, Vol 1 No 3.
- Kandasamy N et al 2016, Children in Care Report Card, Anglicare Victoria.
- Ibid.
- Ibid.
- Mendes P 2009, Improving outcomes for teenage pregnancy and early parenthood for young people in out-of-home care, Youth Studies Australia, Vol 28 No 4, p. 13.
- Ibid.
- Royal Commission into Institutional Responses to Child Sexual Abuse 2017, Volume 12: Contemporary Out-of-home care, Commonwealth of Australia, p. 9.
- Ibid, p. 9.
- Ibid.
- Create Foundation 2018, Create position paper: Young people leaving care as parents, Create Foundation.
- Ibid.
Last updated August 2021
The Australian Bureau of Statistics estimates 14,500 WA young people aged 12 to 17 years (7.9%) had reported disability in 2018.1
Young people living with disability often experience a range of adverse individual and environmental issues, including experiences of discrimination, bullying and exclusion.2 Some disabilities can also make it difficult for young people to communicate, develop supportive social relationships and self-regulate their behaviour.3These difficulties can all increase the risk of young people with disability using alcohol or illicit drugs.
At the same time, young people with disability have the right to explore their gender and sexuality, have relationships based on consent, respect and safety and, where possible, control decisions which affect their sexual health and relationships.4
In 2019, the Commissioner conducted the Speaking Out Survey (SOS19) which sought the views of a broadly representative sample of 4,912 Year 4 to Year 12 students in WA on factors influencing their wellbeing.5 This survey was conducted across mainstream schools in WA; special schools for students with disability were not included in the sample.
In this survey, Year 7 to Year 12 students were asked: Do you have any long-term disability (lasting 6 months or more) (e.g. sensory impaired hearing, visual impairment, in a wheelchair, learning difficulties)? In total, 315 (11.4%) participating Year 7 to Year 12 students answered yes to this question.
Due to the relatively small sample size, the following results for students who reported long-term disability are observational and not representative of the full population of students with disability in Years 7 to 12 in WA. Comparisons between participating students with and without disability are therefore not statistically significant. Nevertheless, these results provide an indication of the views and experiences of young people with disability.
In SOS19 students were asked whether they have ever drunk alcohol (more than just a few sips, like a full can of beer or a glass of wine). Overall, almost one-half (45.6%) of young people in Year 7 to Year 12 with disability reported that they had drunk alcohol, which was a greater proportion than young people without disability (37.5%).
|
Young people with disability |
Young people without disability |
|
|
No |
50.7 |
59.0 |
|
Yes |
45.6 |
37.5 |
|
Prefer not to say |
3.7 |
3.5 |
Source: Commissioner for Children and Young People WA 2020, Speaking Out Survey 2019 Data Tables [unpublished]
Of the young people who had drunk alcohol, similar proportions of young people with disability and without disability had drunk alcohol in the last four weeks (39.3% with disability compared to 41.5% without disability).
One-quarter (24.7%) of young people with disability have tried smoking a cigarette compared to one in five (19.1%) of young people without disability.
|
Young people with disability |
Young people without disability |
|
|
No |
72.3 |
77.7 |
|
Yes |
24.7 |
19.1 |
|
Prefer not to say |
3.0 |
3.3 |
Source: Commissioner for Children and Young People WA 2020, Speaking Out Survey 2019 Data Tables [unpublished]
Of those who have tried smoking a cigarette, young people with disability were more likely to have smoked a whole cigarette (66.6% of young people with a disability compared to 56.9% of young people without a disability).
Similar proportions of young people with disability and young people without disability had had experiences of marijuana. With respect to other drugs, a greater proportion of young people with disability had experiences with other drugs not including tobacco, alcohol or marijuana (18.3% of young people with disability compared to 12.5% of young people without disability).
Research from the United States suggests that young people with disabilities are less likely to smoke, use drugs or drink alcohol at risky levels. However, they also note that young people with emotional disturbances and learning disabilities were more likely to report smoking, drinking and drug use.6
The young people with disability in SOS19 are typically not at the more severe end of the spectrum of disability (as they are attending mainstream schools) and are more likely to have cognitive/learning difficulties and/or behavioural disorders, which aligns with the above research.
Similar proportions of young people with disability in SOS19 compared to young people without, felt they knew enough about alcohol, smoking and other drugs. Although a slightly lower proportion of young people with disability felt they knew enough about the health impacts of alcohol (84.0% of young people with disability compared to 89.0% of young people without disability).
Almost one-third (33.2%) of young people with disability in Year 9 to Year 12 reported that they had been with someone in an intimate or sexual way that included having sexual intercourse. Although not statistically significant due to the sample size, this is greater than the proportion of young people without disability (22.5%).
|
Young people with disability |
Young people without disability |
|
|
No |
61.7 |
70.6 |
|
Yes |
33.2 |
22.5 |
|
Prefer not to say |
5.0 |
6.9 |
Source: Commissioner for Children and Young People WA 2020, Speaking Out Survey 2019 Data Tables [unpublished]
In SOS19, most (91.6%) WA Year 7 to Year 12 students reported that they received some sex education at school. There were minimal differences between young people with disability and young people without disability in what they have been taught at school regarding sex.
All children and young people, regardless of the range of their abilities, must be seen as active and valued citizens who have the right to participate in community life to its full extent. This includes having access to information and resources to make informed choices about alcohol and drugs and their sexuality and sexual and reproductive health.7
Many young people with disability are frequently denied sexual health support and planning due to discrimination, health services being ill-equipped and educated on ability to assist young people with disability and therefore may increase the risk of mistreatment and abuse.8
For information and resource on sexuality and sexual health of people with disability refer to the SECCA website.
Endnotes
- Data is sourced from a custom report provided to the Commissioner for Children and Young People WA by the Australian Bureau of Statistics based on the 2018 Disability, Ageing and Carers survey. The ABS uses the following definition of disability: ‘In the context of health experience, the International Classification of Functioning, Disability and Health (ICFDH) defines disability as an umbrella term for impairments, activity limitations and participation restrictions. In this survey, a person has a disability if they report they have a limitation, restriction or impairment, which has lasted, or is likely to last, for at least six months and restricts everyday activities’. Australian Bureau of Statistics 2019, Disability, Ageing and Carers, Australia, 2018, Glossary.
- National People with Disabilities and Carer Council 2012, SHUT OUT: The Experience of People with Disabilities and their Families in Australia: National Disability Strategy Consultation Report, Australian Government.
- Dix K et al 2013, KidsMatter and young children with disability: Evaluation Report, Flinders Research Centre for Student Wellbeing & Prevention of Violence, Shannon Research Press, p. 15.
- Shine SA 2019, Disability and Sexuality, Shine SA [website].
- Commissioner for Children and Young People WA 2020, Speaking Out Survey: The views of WA children and young people on their wellbeing - a summary report, Commissioner for Children and Young People WA.
- National Center for Special Education Research 2008, Substance Use Among Young Adults With Disabilities, U.S. Department of Education, p. 11
- Sexual Health and Family Planning Australia (SH&FPA) 2013, Improving Sexual and Reproductive Health for People with Disability, SH&FPA Disability Special Interest Group.
- Family Planning NSW 2013, Taking Action on reproductive and sexual health and rights of people with disability: 2014-2018, Family Planning NSW, p. 15.
Last updated August 2021
Most young people in WA engage in positive healthy behaviours, yet participating in experimentation with substances and sexual activity can be part of the transition to adulthood. However, some young people engage in risky behaviours such as the misuse of alcohol or other drugs and unsafe sexual activity. Providing young people with information and support to increase their understanding of the risks involved and how these behaviours can have long-lasting impacts on their health and wellbeing, can enable them to make healthier choices.
Alcohol, tobacco and other drugs
The rates of alcohol, tobacco and other drug use by young people aged 12 to 17 years has declined steadily over the past thirty years in WA. Furthermore, the proportion of young people that reported never having consumed alcohol, tobacco and other drugs has increased.
However, there are a still a significant number of young people drinking alcohol, smoking and taking other drugs at risky levels. For example, for those WA young people who are drinking regularly there has been an increase in the proportion drinking at risky levels on a single occasion.1 Additionally, while drug use overall has decreased over time, the higher quality and lower cost of some drugs (methamphetamine) means those who use illicit drugs are at greater risk of harm.
Research suggests that young people living in remote and regional locations, LGBTI young people and young people in care are more likely to use alcohol, tobacco and other drugs at risky levels. Preventative policies and programs should be targeted to these groups. There also needs to be a concerted effort to improve services and supports for young people who are using alcohol and other drugs at risky levels.
Of particular concern was that one in three WA young people who had consumed alcohol reported sourcing alcohol from their parents. Further to this, research shows that parental drinking behaviour influences the likelihood of young people in their care consuming alcohol. Public health campaigns promoting key messages and harm minimisation strategies are critical, for example, the Alcohol. Think Again campaign which targets parents.
A multifaceted approach is required, which recognises the important role individuals, parents and carers, institutions and communities play in reducing alcohol and drug-related harm. Some key policy priorities should be:
- Strategies that address the broader culture of alcohol consumption in Australia. Programs should be delivered to involve and educate parents and the wider community recognising that social influence, particularly from parents and peers, has a significant impact on young people’s behaviours. Provide a supportive environment for parents’ behavioural change, reinforced in external environments such as schools, sporting clubs and the media.
- Compulsory culturally appropriate education on alcohol, smoking and drugs in schools. Promoting protective behaviours and a positive school culture is a key component of this approach. School-based alcohol, smoking and drug education programs should aim to modify behaviour, not just increase knowledge and competence.
- Listening to young people’s experiences with alcohol, tobacco and drugs is critical to developing effective policy. Young people should be an integral part of the ongoing development and implementation of strategies to reduce alcohol and drug-related harm.
- Policy makers and educators should consider the unique developmental period of the middle years (nine to 14 year olds) as the stage to commence age-appropriate school-based alcohol, smoking and drug education programs.
- Reduce the availability of cheap and discounted alcohol, through means such as volumetric taxation and/or introduction of a minimum floor price.
- Consider legislation to restrict the advertising and promotion of alcohol, particularly advertising to which children and young people are exposed (e.g. billboard and sport advertising).
- Provision of more alcohol-free events for children, young people and families.
- Providing accessible, holistic, culturally appropriate family-focused treatment services that assess and meet the needs of children and young people living with parents who have an alcohol or drug dependency.2
For further information on young people and alcohol refer to the following:
Commissioner for Children and Young People WA 2018, Policy Brief: Alcohol and the role of parents, Commissioner for Children and Young People WA
Sexual health
It is important for young people to grow and develop in a supportive social environment. Strong relationships with parents, peers and the school community all assist in establishing a supportive social environment for young people throughout their sexual development.
Across Australia, two in three young people aged 15 to 17 years of age have reported experiencing some form of sexual activity (deep kissing, genital touching, oral sex or penetrative sex). Of young people engaging in sexual activities, more than half are at risk of contracting a sexually transmissible infection due to unsafe sexual practices. Research has also highlighted that young people aged 15 to 17 years across Australia have limited knowledge of STI transmission.3
Improving the knowledge and understanding of young people about sexual health is critical and should be a focus of policy and sexual health education within all schools. Research clearly shows that educating young people about sex and sexual health does not encourage young people to engage in sexual activities earlier.4
Policy, programs and education also need to recognise and support the diversity of young people’s sexual identities and experiences.
Sexual health includes not only safe sex practices to reduce the risk of sexually transmissible infections (STIs), but should also include appropriate access to information and services that are inclusive, culturally safe and address healthy relationships, sexual coercion and consent.
Female young people are particularly at risk of experiencing unwanted or coercive sexual experiences which can influence their self-esteem, mental health and wellbeing more broadly. Early and age-appropriate education which supports children and young people’s understandings of healthy and respectful relationships and consent is essential.
The rates of births to WA female young people 17 years and under has decreased steadily over the last 12 years. However, factors such as limited access to high quality and culturally safe health care services, poor sexual health education, poverty and living in remote and regional areas increase the likelihood of risky behaviours which could lead to a young person becoming a teenage parent.
Some key policy priorities to improve young people’s sexual health knowledge and practice should include:
- Compulsory diverse and inclusive (gender, age, cultural and linguistic backgrounds, socio-economic status, sexual orientation, disability and geographic location) sexual health education should be provided in high schools.5 The WA Department of Education’s, Growing and Developing Healthy Relationships program provides guides and learning tools.
- Policy makers and educators should also consider the unique developmental period of the early middle years (nine to 11 years) as the stage to commence age-appropriate school-based sexual health and respectful relationships education programs.6
- Recognising that parents and communities are critical influences on children and young people’s knowledge and understanding of sexual health issues, culturally appropriate resources for parents and communities should be widely disseminated. For example, the WA Department of Health publishes the Talk soon. Talk often guide to help parents talk to their children about sex.
- Improving access to sexual health services, particularly for young people in regional and remote areas. This may include outreach sexual health education, programs and clinical services.
- Encouraging the use of condoms during sexual activity is critical.7 Free or low cost condoms should be available and accessible across the whole state.
- Promoting safe sex behaviours including understanding consensual sex and the importance of regular STI testing.
- Young people should be an integral part of the ongoing development and implementation of strategies and programs pertaining to their sexual health education and support.
Young people experiencing vulnerability, in particular young people in care and in the youth justice system are at an increased risk of engaging in unsafe sexual activities. Yet, they have often had less access to sexual health education and services. Sexual health education and access to condoms and sexual health services should be prioritised for these groups.
All young people are different and while membership of one of any groups is influential (e.g. LGBTI, Aboriginal or living in a remote location etc.), there are many other factors which influence a young person’s identity and experiences. Thus, policy and programs need to not only recognise the heightened risk for different groups, but also be person-centred and focused on the needs and circumstances of the individual.
Data gaps
There has been a welcome increase in the availability of data on the prevalence of consumption of alcohol, tobacco or other drugs, and the sexual health of WA children and young people.
However, little data is available on alcohol consumption or other drug use for Aboriginal children and young people in WA. This is a critical gap. Multiple inquiries have highlighted the need for further programs and services to support Aboriginal children and young people with drug and alcohol issues.8,9 To inform planning and implementation of these recommendations it is essential that data is collected and reported on the prevalence of alcohol and other drug issues for Aboriginal children and young people in WA.
The Australian Study of Health and Relationships (ASHR) survey is conducted every ten years and provides a snapshot of the sexual health and wellbeing of the Australian population.10 However, this data is often too old to be relevant and is not available to the general public.
The National Survey of Australian Secondary Students and Sexual Health is a survey that is conducted every five years that collects the sexual attitudes, knowledge and experiences of high school students in Years 10 to 12 across Australia. Although this study is completed more frequently, the study only includes attitudes, knowledge and experiences of young people in Years 10 to 12 and only those that attend high schools.
Considering many young people are engaging in sexual activity before they reach Year 10, it is essential to understand their experiences and knowledge in this area. This information is critical for the planning/service delivery/education programs that specifically relate to the sexual health needs of WA young people.
LGBTI status, unlike other demographic characteristics, are not readily identifiable through existing data collection methods (such as coronial records, surveys, administrative data collected by services).10 The lack of data on the prevalence of alcohol and other drug use and sexual health issues for LGBTI children and young people makes it difficult to effectively improve services and supports for them.
There is no data publicly available on the prevalence of alcohol and other drug use and sexual health issues among WA young people in out-of-home care or the youth justice system, even though it is well known these young people are vulnerable and at high risk of risky behaviours such as alcohol and drug use and unsafe sexual activities.
The limited data being collected and reported regarding alcohol and other drug use and sexual health of WA young people from refugee and migrant backgrounds is of concern. With refugee young people potentially dealing with trauma, conflict and settlement issues, the use of alcohol and other drugs can become a way of coping. In addition, with migration comes breakdowns in families, disconnection from peers, and inconsistencies in education, which mean that sexual health education may not be a primary focus in many of these families’ lives.
More research and data is required to understand both alcohol and drug use and sexual health attitudes and experiences of young people with disability. All children and young people, regardless of the range of their abilities, must be seen as active and valued citizens who have the right to participate in community life to its full extent and without such data it makes it difficult to effectively improve services and supports for this cohort.
Endnotes
- Mental Health Commission (MHC) [undated], Alcohol trends in Western Australia: Australian school students alcohol and drug survey, MHC.
- Commissioner for Children and Young People WA 2011, Speaking out about wellbeing: children and young people speak out about alcohol and drugs, Commissioner for Children and Young People WA.
- Mitchell A et al 2014, 5th National Survey of Australian Secondary Students and Sexual Health 2013, Australian Research Centre in Sex, Health and Society, La Trobe University, p. v.
- UNESCO 2009, International Technical Guidance on Sexuality Education: An evidence-informed approach for schools, teachers and health educators, Volume 1: the rationality for sexuality education, UNESCO, p. 8.
- Skinner R and Hickey M 2003, Current priorities for adolescent sexual and reproductive health in Australia, The Medical Journal of Australia, Vol 179 No 3.
- UNESCO 2009, International Technical Guidance on Sexuality Education: An evidence-informed approach for schools, teachers and health educators, Volume 1: the rationality for sexuality education, UNESCO, p. 8.
- Department of Health 2019, Perspectives on working with young people: A youth health issue in focus: young people, sex and pregnancy [website].
- Education and Health Standing Committee: WA Parliament 2016, Learnings from the message stick: The report of the Inquiry into Aboriginal youth suicide in remote areas, WA Government.
- WA State Coroner 2019, Inquest into the deaths of: Thirteen children and young persons in the Kimberley region, Western Australia, WA Government.
- Australian Study of Health and Relationships (ASHR) 2014, Sex in Australia 2 – Summary, The University of NSW, The University of Sydney, University of Sussex and La Trobe University.
- Rosenstreich G 2013, LGBTI People Mental Health and Suicide, Revised 2nd Edition, National LGBTI Health Alliance, p. 6
For further information on the healthy behaviours of young people refer to the following resources:
- Hill A et al 2021, Writing Themselves In 4: The health and wellbeing of LGBTQA+ young people in Australia - National report, La Trobe University.
- Justice Health & Forensic Mental Health Network and Juvenile Justice NSW 2015, 2015 Young People in Custody Health Survey: Full Report, NSW Government.
- Kandasamy N et al 2016, Children in Care Report Card, Anglicare Victoria.
- Fisher CM et al 2019, National Survey of Australian Secondary Students and Sexual Health 2018, ARCSHS Monograph Series No. 113, Australian Research Centre in Sex, Health & Society, La Trobe University.
- Office of Multicultural Interests 2009, Not drowning, waving: Culturally and linguistically diverse young people at risk in Western Australia, WA Government.
- Shine SA 2019, Disability and Sexuality, Shine SA [website].
- WA Mental Health Commission 2020, Bulletin: Illicit drug trends in Western Australia: Australian school students’ alcohol and drug survey - 2017, WA Government.
- Ward J et al 2020, The Goanna Survey 2: Results of the second Australian survey of knowledge, relationships, behaviour and health service access relating to sexually transmissible infections (STIs) and blood borne viruses (BBVs) among Aboriginal and Torres Strait Islander young people, The Kirby Institute, University of New South Wales.
Endnotes
- Australian Institute of Health and Welfare (AIHW) 2011, Young Australians: their health and wellbeing 2011, Cat no PHE 140, AIHW.
- Ibid, p. 80.
- Australian Institute of Health and Welfare (AIHW) 2016, Australia’s health 2016 – Chapter 5.4 Health of young Australians, Australia’s health series no 15, Cat no AUS 199, AIHW.